Assessing Postpartum Bleeding
Diana is a healthy 35-year-old G5P5 who vaginally delivered an 8 pound, 6 ounce baby girl with an intact perineum. Her estimated blood loss (EBL) was 500 mL. During the fourth stage of labor her vital signs, fundus, and lochia were within normal limits (WNL). She is transferred to the mother-baby unit 3 hours after birth.
- What is the postpartum period?
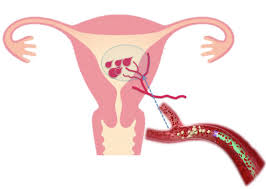
- What is the process of uterine involution after childbirth?
- How is postpartum hemostasis achieved?
- After the report, the nurse goes in to assess Diana. Her vital signs are WNL, but her fundus is 2 cm above the umbilicus and displaced to the right. Her sanitary pad is completely saturated with lochia rubra. Is this an expected finding 3 hours after birth?
- The nurse asks Diana to dangle her feet at the bedside for several minutes. After confirming that Diana does not feel dizzy or lightheaded, she helps Diana up to the bathroom to void. Why does the nurse think that Diana’s bladder is full?
- When Diana first gets out of the bed, she has a gush of blood. Is this a sign of hemorrhage?
- Diana voids 500 mL of urine. Her fundus is boggy but became firm with massage and is now at the level of the umbilicus. Her lochia flow is slightly decreased. Diana has an IV of lactated Ringer (LR) solution with 20 units of oxytocin infusing at 125 mL per hour. What else can the nurse do to help Diana’s uterus contract?
We can write this or a similar paper for you! Simply fill the order form!




