Transitional Management for Adult Patients of Chronic Obstructive Pulmonary Disease (COPD)
Order Instructions:
Using APA format ,write six (6) to ten page paper (excludes covers and references pages) that addresses the disease management needed of adult patients with COPD for a safe transition between the acute care setting and home and the role of the interdisciplinary team in that transition.
SAMPLE ANSWER
Transitional Management for Adult Patients of COPD
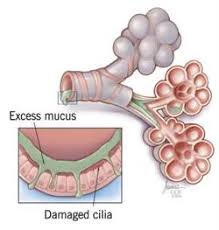
Chronic Obstructive Pulmonary Disease (COPD) is an incurable medical condition that is more prevalent in older people than in the young. Even though COPD is incurable, it is possible to minimize the severity of its symptoms by structuring optimal management techniques. Such practices should minimize the rate of disease progress and offer patients a chance to lead high-quality lives. However, it is often challenging to ensure that patients receive optimal management for the disease, more so when they are leaving acute care centers for their homes. There are important approaches to consider in ensuring that patients practice the recommended strategies for managing COPD at their homes. The activity would involve an interdisciplinary collaboration between professionals in the healthcare setup.
Part 1: The Use of Bronchodilators and Corticosteroids in the Management of COPD
- Why They are Used
Bronchodilators and corticosteroids are effective in the alleviation of clinical symptoms of COPD. Bronchodilators such as salmetrol, formoterol, and tiotropium work on a long-term basis to enhance lung functionality and reduce the occurrence and severity of exacerbations, hence improving patient’s quality of life. The drugs also enhance patient’s tolerance to exercises and improve protect them from lung hyperinflation as well as dyspnea (Tashkin, & Ferguson, 2013). Drugs such as indacaterol and aclidinium are new developments that require less dosage frequencies hence reducing chances of drug non-adherence among patients. Other bronchodilators with lengthy frequencies of intake include glycopyrrolate, vilanterol, and olodaterol (Tashkin, & Ferguson, 2013).
Corticosteroids are also important medications in the management of exacerbations experienced in COPD. Nebulized budesonide is not only a primary care corticosteroid in managing OCPD in adults, but it is also the drug of choice for children with COPD. Clinicians prefer the drug on the basis of its considerably less severe side effects compared to those associated with the use of other steroids (Gaude, & Nadagouda, 2010, Pg. 230). Timely administration of corticosteroids also results in improved functionality of the lungs. Some glucocorticoids also find use in reducing inflammation. They act by inhibiting the genetic pathway leading to the production of inflammatory mediators such as chemokines and cytokines (Gaude, & Nadagouda, 2010, Pg. 231). Instead, they promote the production of anti-inflammatory molecules such as beta-2 adrenoceptors. Through such a mechanism, glucocorticoids reduce swelling and exudation on the airway hence enhancing the respiratory system.
- Side Effects of Corticosteroids and Bronchodilators
The use of corticosteroids has adverse effects such as sleep abnormalities, exaggerated appetite, and weight gain. They also subject adult users to ailments such as osteoporosis, diabetes, pneumonia, hypertension, cardiac anomalies, cataracts, and peptic ulcers (Gaude, & Nadagouda, 2010, Pg. 232). The side effects are severer when patient are on oral and parenteral treatment with corticosteroids as compared to when they take inhaled and nebulized formulations. The prevalence of the undesirable effects also increases with the dosage amount. Bronchodilators also have associated adversities. They include muscle crumps, headache, dizziness, nausea, vomiting, palpitations, and cardiac abnormalities (Cleveland Clinic, 2014a). Patients should report severe critical side effects so that prescribers can substitute their regimens with others that have minimal adversities. Occurrences such as hypertension, severe headaches, persistent vomiting are worth reporting as they may indicate the development of other critical conditions such as cardiac diseases and peptic ulcers. Patients may not have to report effects such as dizziness, nausea, and minor headaches as such complications are common with most medications. Besides, such symptoms are often temporary, and they would rarely indicate serious clinical adverse conditions.
- Special Instructions Regarding Drug Use
Both bronchodilators and corticosteroids require special directions for their use. For instance, health professionals should advise their patient to take bronchodilators before taking other inhaled medications such as corticosteroids. Again, it is important to inform patients that they do not have to chew bronchodilator tablets, and instead, they should swallow them as whole. It is also necessary to inform patients on the purpose of each medication. For instance, patients should know that bronchodilators help them overcome shortness of breath associated with COPD. Some of the additional directions also apply to the use of corticosteroids. For instance, patients would always require taking bronchodilators first when they are co-administered with steroids. For corticosteroids, patients should know that they require rinsing their mouth with clean water to minimize the occurrence of side effects such as nausea. Also, it is important to inform the patient that unlike bronchodilators, corticosteroids take a considerably longer time to work, and they are not applicable for instant relief of COPD symptoms. Again, patients should know that corticosteroids may not stop attacks that have already started (Cleveland Clinic, 2014b).
- An Important Healthcare Discipline that would Facilitate Medication Adherence
Medication adherence entails the degree of compliance with the recommended drug use practices. So as to ensure optimal treatment adherence among patients, various healthcare disciplines should collaborate. Among such disciplines are the nursing and pharmacy departments. Nurses have most interactions with patients as their primary role is to monitor patients. On the other hand, pharmacists are the custodians of drug use, and they would be relevant in promoting adherence to medications. Pharmacists should cooperate with nurses to schedule follow up activities to monitor drug use among patients (Jimmy, & Jose, 2011, Pg. 156). They should for instance establish strong interactions with patients, teach them on how to use devices such as inhalers, and monitor their use of adherence devices such as calendars and reminders.
Part 2: Dietary Modification in the Management of COPD
- The Role of Diet in Managing COPD
Diet is a crucial consideration in the management of COPD. Either form of malnutrition, be it excessive nutrient consumption, or low intake of the same has an undesirable impact on the pathogenesis of COPD. Dieting habits that promote the development of conditions such as obesity have severe impact on COPD development. Usually, obesity leads to other respiratory abnormalities that worsen the condition of COPD patients. Such illnesses include asthma, hypoventilation, and pulmonary embolism (Hanson, Rutten, Wouters, & Rennard, 2014, Pg. 724). On the other hand, COPD patients with advanced disease experience pulmonary cachexia, a state in which their body weight is abnormally low, and their free fatty mass is extremely reduced.
Dietary modifications would be necessary to enhance the nutritional status of patients. Malnourished COPD patient would have to rely on dietary supplements to boost their health. Alternatively, patients would have to include high-calorie foods and beverages in their dietary plans. Studies indicate that lean COPD patients should maximize their fat intake at the expense of carbohydrates (Itoh, Tsuji, Nemoto, Nakamura, & Aoshiba, 2013, Pg. 1318). Some cultures encourage consumption of meat while others discourage it. Likewise, cultures have varying influences regarding intake of fruits and vegetables.
- Possible Obstacles to Dietary Modification
Patients may find it hard to adopt new dietary practices. Also, people’s living conditions may influence their ability to adopt certain therapeutic dietary approaches. Patients from poor economic backgrounds may not access the recommended dietary practices. Cultural beliefs may also influence the adoption of dietary changes. Some cultures may not encourage certain recommended dietary approaches. Patients’ taste and preferences may also hinder the adoption of dietary changes. Some nutrients are only abundant in foods that some patients may be unwilling to take. Such foods include fish and mushrooms, both which are sources of vitamin D, an element crucial for COPD patients (Itoh et al., 2013, Pg. 1320).
- An Important Healthcare Discipline in Facilitating Dietary Modifications
Nurses should seek the collaboration of dieticians in promoting effective dietary modifications. COPD patients experience important nutritional complications such as appetite loss. Medical dieticians are best placed to inform patients on practices that would promote their appetite. They should offer nutrition therapy to protect patients from weight loss and attacks by COPD Comorbidities (Seo, 2014, Pg. 151). Likewise, the professionals would advise obese persons on measures they should take to avoid worsening their health status. Dieticians should also collaborate with the families of patients by advising them on the foods that their patients may need as well as the ones they should avoid.
Part 3: Physical Activity in COPD Management
- The Role of Physical Activity in COPD Management
While it is advisable for people to engage in physical exercises, COPD patients should maintain their level of involvement to a certain level. Too much strenuous activities may have adverse consequences in the population. The pathophysiology of COPD involves dyspnea, a condition that may worsen with engagement in exercises. Simple exercises are however necessary to ensure that patient’s respiratory system is strengthened. Energy conservation is crucial in COPD patients both in the sense that the victims could easily ran malnourished and also considering the appropriate management of dyspnea. Recommended physical exercises for the group include diaphragmatic and pursed-lip forms of breathing techniques (Broward Health, 2015). COPD patients also require physical exercises for psychological health. There are multiple factors that would predispose the group to stress, depression, and anxiety. The knowledge of having a chronic ailment is among such factors. Also, experiences of dyspnea and its associated discomfort would easily trigger anxiety. Patient would need keeping themselves busy through exercises so as to overcome such events.
- The Role of RN in Promoting Effective Physical Practices in COPD Management
Registered nurses prioritize on the welfare of patients. They should structure an exercise strategy that would not harm but benefit patients. They would do so by warning patients against engagement in strenuous activities and advise them on appropriate activities they should explore. Nurses should also monitor the performance of their patients to help them maintain healthy physical conditions. Nurses should educate patients on activities that would promote their pulmonary system. Such advice should also entail practices that patients should engage in so as to overcome symptoms such as dyspnea. Also, nurses should advise patients on relaxation strategies that would promote healthy air flow in their systems.
- An Essential Healthcare Discipline in Facilitating the Healthy Physical Activities
Physical therapists would be relevant professionals in enhancing the effectiveness of physical activity in the management of COPD patients. The specialists should collaborate with nurses in ensuring that COPD patients are at their optimum physical health. Physical therapists should teach patients on how to perform various exercises in a safe manner. COPD patients often have a delicate physical health, and the specialists should purpose to promote their (patients’) stability. Also, it is important for physical therapists and nurses to engage patients’ family members in strategizing physical activities for their patients. They should encourage patients’ family members to support their loved ones in exercising. Families would do so by monitoring their patients as they engage in various activities. They could also contribute by helping patients to undertake manual activities that could otherwise trigger hypoventilation and dyspnea in the high-risk group.
Part 4: Conclusion
- The Effectiveness of an Interdisciplinary Team in Managing COPD
It is important to maintain the quality of care for COPD patients at a high level, especially during transitions from hospital care to home-based attendance. The process involves various considerations ranging from medication adherence, dietary practices, and the performance of physical activities. As such, the process would require various clinical professionals to cooperate for high-quality outcomes. Engaging nursing care and other relevant specialties in the transition would be a promising move. The team should work jointly with the common goal of bettering patient outcomes. A team involving specialties from the most relevant departments and professions would be effective in achieving utmost patient satisfaction and fetching desirable outcomes. It is also vital that such a team involve the families of patients. The extent of patient satisfaction would be a reflection of the ultimate achievements of the interdisciplinary team involved in the entire process.
References
Broward Health. (2015). Struggling to breath: tips for managing dyspnea. Retrieved from http://www.browardhealth.org/Taxonomy/RelatedDocuments.aspx?sid=1&ContentTypeId=34&ContentID=21274-1
Cleveland Clinic. (2014a). Fast acting bronchodilators for COPD. Retrieved from http://my.clevelandclinic.org/health/diseases_conditions/hic_Understanding_COPD/hic_Pulmonary_Rehabilitation_Is_it_for_You/hic_fast_acting_bronchodilators_for_copd
Cleveland Clinic. (2014b). Anti-inflammatory medications for COPD. Retrieved from http://my.clevelandclinic.org/health/diseases_conditions/hic_Understanding_COPD/hic_Pulmonary_Rehabilitation_Is_it_for_You/hic_anti-inflammatory_medications_for_copd
Gaude, G. S., & Nadagouda, S. (2010). Nebulized corticosteroids in the management of acute exacerbation of COPD. Lung India : Official Organ of Indian Chest Society, 27(4), 230–235. http://doi.org/10.4103/0970-2113.71957
Hanson, C., Rutten, E. P., Wouters, E. F., & Rennard, S. (2014). Influence of diet and obesity on COPD development and outcomes. International Journal of Chronic Obstructive Pulmonary Disease, 9, 723–733. http://doi.org/10.2147/COPD.S50111
Itoh, M., Tsuji, T., Nemoto, K., Nakamura, H., & Aoshiba, K. (2013). Undernutrition in Patients with COPD and Its Treatment . Nutrients, 5(4), 1316–1335. http://doi.org/10.3390/nu5041316
Jimmy, B., & Jose, J. (2011). Patient Medication Adherence: Measures in Daily Practice. Oman Medical Journal, 26(3), 155–159. http://doi.org/10.5001/omj.2011.38
Seo, S. H. (2014). Medical Nutrition Therapy based on Nutrition Intervention for a Patient with Chronic Obstructive Pulmonary Disease. Clinical Nutrition Research, 3(2), 150–156. http://doi.org/10.7762/cnr.2014.3.2.150
Tashkin, D. P., & Ferguson, G. T. (2013). Combination bronchodilator therapy in the management of chronic obstructive pulmonary disease. Respiratory Research, 14(1), 49. http://doi.org/10.1186/1465-9921-14-49
We can write this or a similar paper for you! Simply fill the order form!




