Liver disease
Order Instructions:
select only one (1) of the case studies provided :
• Remember this is an essay and should be structured as such with an introduction body and conclusion. Do not simply answer the questions provided, these are given as a guide. You will be expected to use research or evidence-based journal articles, textbooks and appropriate authoritative web sites (not Better Health Channel, Virtual Hospital, etc.).
• All referencing is to be formatted using the APA referencing style. Please ensure carefully to follow the marking criteria
SAMPLE ANSWER
Liver disease
Introduction
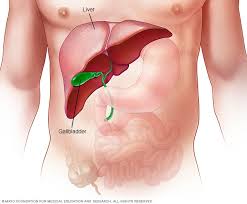
Alcohol is a hepatotoxic compound that is commonly consumed across the globe. It is linked to a broad range of liver associated injury, ranging from simple steatosis, fibrosis to cirrhosis (Torruellas, French, & Medici, 2014). Alcohol liver disease refers to a spectrum of alcohol-related injuries that are potentially reversible especially when the progression of the disease is detected early enough. Therefore, regular screening and early diagnosis are essential. Excessive alcohol consumption adversely affects the health of an individual and is one of the primary causes of death in the world. Harmful or excessive use of alcohol results in a mortality rate of up to 2.5 million and an approximate disability of adjusted life years of up to o 69.4 million (Shield, Parry, & Rehm, 2013). As a result, it has been ranked as one of the leading risk factors for death and disability worldwide. The toxicity of alcohol components including ethanol largely contribute to increased chances of developing liver disease. The liver controls most of the body support systems, therefore, a disease of the liver is fatal as it will lead to malfunction of all the major body systems
Causes of confusion and other symptoms.
Various factors contribute to the occurrence of liver disease. Of these, duration and amount of alcohol consumed are most significant. Host factors such as IPNPLA3 gene polymorphisms and obesity and environmental factors also contribute to an increased risk of developing liver disease (Singal, Chaha, Rasheed, & Anand, 2013). Disease of the liver leads to reduced functionality of the liver which consequently cause accumulation of toxic substances in the bloodstream. These instances lead to alterations in the level of consciousness of an individual, confusion, and other cases coma. In Mr. McGrath’s case, hepatic encephalopathy may be the cause of disorientation.
Abdominal swelling by the patient indicates extensive complications. Life-threatening complications associated with portal hypertension including ascites may be present in the patient. Increased pressure on the portal vein leads to ascites characterized by fluid build-up in the abdominal cavity. Yellowish skin, delirium, and confusion are also observed in this condition (A.D.A.M, 2013). Varices are likely to develop in instances of portal hypertension, as a means of providing alternative pathways for diverted blood.
Oesophageal varices pathophysiology and management strategies.
Almost half of the patients suffering from cirrhosis during diagnosis have been found to have gastroesophageal varices (Pericleous et al., 2016). The varices arise due to portal hypertension resulting from an increase in portal blood flow resistance in cirrhosis and also due to the rise in blood inflow into the portal vein. An increase in resistance is said to be structural, due to a destruction of the vascular architecture of the liver by regenerative nodules and fibrosis as a result of an increase in the tone of the hepatic vasculature primarily due to the dysfunction of the endothelium and a decrease in the bioavailability of nitric oxide.
Three principal events cause portal hypertension. First, it can be due to a physical obstruction arising from a fibrosis or at other instances from regenerative nodules resulting in an increase in the resistance to blood flow. An imbalance between vasoconstrictors and vasodilators in the liver also develops. Such imbalance results in a reduction of the activity of eNOS in the liver. The event is, however, rectifiable using medications such as nitrates and beta-blockers. A combination of these events leads to the occurrence of porto-systemic collateral circulation of aiming to decompress the portal circulation (Frazier, Stocker, Kershner, Marasano, & McClain, 2014). Splanchnic vasodilation occurs due to a relative extra-hepatic and ischaemic liver increase in Nitrite Oxide, with the signalling of the sGC-PKG and smooth muscle cell relaxation. This leads to increased blood flow volume into the portal which maintains hypertension. This results in a hyper-dynamic circulation that is linked to these hemodynamic variations in portal hypertension and cirrhosis. This is manifested as high cardiac output with little arterial hypotension and systematic vascular resistance (Pericleous, et al., 2016).
Hepatic pressure can be applied to obtain hepatic venous pressure gradient (HVPG) that ranges normally from 1 to 5mmHg. This procedure is performed by inserting a catheter into a hepatic vein to get the hepatic vein pressure. HVPG is equal to WHVP minus free (HVP) where HVPG is used to represent the gradient between caval pressure and the portal (Molina et al., 2016). FHVP acts as an internal zero by cancelling out variations in abdominal pressure. Sinusoidal hypertension differs from pre-sinusoidal portal hypertension which associated with an increase in HVPG as flow resistance builds up in the portal vein. Varices therefore develop in the event that HVPG is greater than ten mmHg.
Antibiotics have been introduced in variceal hemorrhage management, a factor which has significantly improved clinical outcomes. Bacterial infections, both primary and secondary, are common in cirrhotic patients as bacteria actively translocate from the impaired mucosal surface into the portal system and the patient’s impaired immune function (Molina, Gardner, Souza-Smith, & Whitaker, 2014). In these patients, antibiotics decrease the bacterial load, reducing infections, recurrent bleeding, and reduce morbidity and mortality in patients with gastroesophageal varices. Broad spectrum antibiotics prophylaxis is thus recommended in individuals with suspected and confirmed variceal hemorrhage (Shah, 2016).
Nonselective beta blockers can be used in patients having a low-risk small varices, as they can delay variceal growth preventing variceal bleeding (Runyon, 2015, September 23). The treatment is applied in absence of severe liver disease, and where the varices are without red wale marks. In persons with varices containing red wale marks and others associated with a high risk of haemorrhage, non-selective beta-blockers are used.
For patients that have medium and large varices, endoscopic variceal ligation or beta-blockers can be used. Non-selective beta-blockers are advantageous as they are cheap and use requires no expertise. These medications also prevent against other medical conditions like spontaneous bacterial peritonitis and bleeding from ascites and portal hypersensitive gastropathy (Garcia-Tsao & Bosch, 2011).
The role of abdominal paracentesis and possible complications.
The presence of excess fluid in a patient’s abdominal cavity cause significant discomfort to the patient and shortness of breath. Abdominal paracentesis is a simple procedure that involves insertion of a needle into the peritoneal cavity of the patient to remove the ascetic acid. Removal of a small amount of the fluid for testing is referred to as diagnostic paracentesis, while therapeutic paracentesis is considered the removal of up to five litres of the excess fluid so as to decrease the resultant intra-abdominal pressure helping in relieving related abdominal pain, dyspnea and early satiety (Runyon, 2015).
Paracentesis should be performed by a properly trained physician. Performing this procedure at the time the patient is admitted to a hospital, to patients suspected or suffering from cirrhosis and ascites decrease the mortality rates in a health care setting. In instances where paracentesis was conducted on admission, a lower in-hospital mortality rate was recorded compared to those who did not perform the procedure (Cavazzo, Bugiantella, Graziosi, Franceschini, & Donini, 2013).
Paracentesis also helps clarify the primary cause of ascites when testing for infection. Unexpected diagnoses including chylous, eosinophilic or hemorrhagic ascites can also be indicated by this procedure (Pericleous et al., 2016). Analysis of the fluid shed light on the cause of the ascites and if present, the bacterial infection. Upon culturing antibiotic susceptibility of the bacteria can be identified therefore easier treatment.
Despite the benefits of paracentesis, various complications occur. The ascitic fluid leak is the most common complication associated with the procedure. Failure to peform a Z-track properly can lead to a leakage of the ascetic fluid leak. In this case, a large-bore needle may be used, or when the skin incision created is overly large. If the leak on the surface is prolonged, cellulitis may develop (Wedro, 2015).
Bleeding from a blood vessel may arise if a vein or artery is torn by the needle. Bleeding can be extremely severe and potentially fatal especially if an artery is affected. A further disastrous situation may arise in the presence of renal failure. In patients with primary fibrinolysis, three-dimensional hematomas may develop requiring anti-fibrinolytic treatment (Molina et al., 2014). Bowel infection may occur in instances where the bowel has been injured by the paracentesis needle. Fortunately, this does not usually result to clinical peritoritis, and thus treatment is not necessitated, not unless patients indicate signs of infections. Death may also occur due to paracentesis.
Mr. McGrath educational requirements.
Mr. McGrath should be advice on the importance of total abstinence from alcohol to prevent further complications. He should also be educated to take a diet low on ammonia to reduce the amount of toxic products that will be produced by the body. High cholesterol containing foods should also be avoided to reduce the arterial pressure and therefore amount of fluid in the stomach. The prescribed medicine should be strictly adhered to prevent further complications. Garcia-Tsao & Bosch, (2011) enlighten that support groups and peer help especially from other patients and medical practitioners can be employed to provide additional moral support to patients. Sharing of past experiences by the patients will boost the recovery of Mr. McGrath. Mr.Grath should be advised on the importance of abstinence from cigarettes as they significantly increase the level of toxic compounds in his blood system.
Analysis of Mr. McGrath current prescription.
Propranolol or otherwise known as Inderal is prescribed to the patient for pharmacologic crophylaxis of variceal bleeding. Varices may probably have been identified in the patient. Propranolol reduces the portal pressure through reduction in the cardiac output, and reducing portal blood inflow via splanchnic vasoconstriction (Runyon, 2015, September 23). Spironolactone is an aldosterone antagonist which act on the distal tubules to conserve potassium and increase natriuresis. The drug is mainly used as a diuretic. Furosemide is prescribed to Mr. McGrath to treat the fluid build-up in the body. The drug is an anthranilic acid derivative and a diuretic. It inhibits absorption of sodium and chloride in the proximal, the loop of Henle and distal tubes.
Conclusion
Alcohol liver disease is one of the primary causes of liver-related mortality in the United States. Clinicians, therefore, should be well versed in diagnosis and treatment procedure for the condition. Education to the population may play a significant role in reducing severe forms of the conditions by advocating for early testing and treatment. In Mr McGrath case, follow-up after treatment should be conducted to facilitate a full recovery. In cases of total failure of the liver a transplant should be considered in order to maintain the acceptable toxicity levels of blood ammonia.
References
A.D.A.M (Ed.). (2013, December 23). Cirrhosis. Retrieved September 4, 2016, from The New York Times: http://www.nytimes.com/health/guides/disease/cirrhosis/possible-complications.html
Cavazzo, E., Bugiantella, W., Graziosi, L. A., Franceschini, M. S., & Donini, A. (2013, February). Malignant ascites: pathophysiology and treatment. International Journal of Clinical Oncology, 18(1), 1-9. doi:10.1007/s10147-012-0396-6
Frazier, T. H., Stocker, A. M., Kershner, N. A., Marasano, L. S., & McClain, C. J. (2014, May 1). Critical pathophysiological process and contribution to disease burden. Physiology, 203-215. Retrieved September 04, 2016
Garcia-Tsao, G., & Bosch, J. (2011, March 4). Management of varices and variceal hemorrhage in cirrhosis. The New England Journal of Medicine, 362, 823-832. doi:10.1056/NEJMra0901512
Molina, P. E., Gardner, J. D., Souza-Smith, F. M., & Whitaker, A. M. (2014). Alcohol abuse: Critical pathophysiological processes and contribution to disease burden. Physiology, 29, 203-215. doi:10.1152/physiol.00055.2013
Pericleous, Marinos, Sarowski, Alexander, Moore, Alice, . . . Murtaza. (2016, March). The clinical management of abdominal ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome: a review of current guidelines and recommendations. European Journal of Gastroenterology & Hepatology, 28(3), e10-e19. Retrieved September 04, 2016, from http://www.ingentaconnect.com/content/wk/ejghe/2016/00000028/00000003/art00001?crawler=true
Runyon, B. A. (2015, September 23). Diagnostic and therapeutic abdominal paracentesis. Retrieved September 04, 2016, from UpToDate: http://www.uptodate.com/contents/diagnostic-and-therapeutic-abdominal-paracentesis
Shah, R. (2016, August 24). (P. K. Roy, Editor) Retrieved September 04, 2016, from http://emedicine.medscape.com/article/170907-treatment
Shield, K. D., Parry, C., & Rehm, J. (2013). Focus on: Chronic diseases and conditions related to alcohol use. The Journal of National Institute on Alcohol Abuse and Alcoholism, 35(2). Retrieved September 4, 2016, from http://pubs.niaaa.nih.gov/publications/arcr352/155-173.htm
Singal, A. K., Chaha, K. S., Rasheed, K., & Anand, B. S. (2013, September 28). Liver transplantation in alcoholic liver diseases current status and controversies. World Journal of Gastroenterology, 19(36), 5953-5963. doi:10.3748/wjg.v19.i36.5953
Torruellas, C., French, S. W., & Medici, V. (2014, September 7). Diagnosis of alcoholic liver disease. World Journal of Gastroenterology, 20(33), 11684-11699. doi:10.3748/wjg.v20.i33.11684
Wedro, B. (2015, July 28). Medical treatment. (M. C. Stoppler, Editor) Retrieved September 04, 2016, from E medicine health: http://www.emedicinehealth.com/ascites/page7_em.htm
We can write this or a similar paper for you! Simply fill the order form!




