Evidence based research on Prophylactic antibiotic timing and SSIs incidences
Order Instructions:
Please follow the instruction attached.
SAMPLE ANSWER
Prophylactic antibiotic timing and SSIs incidences
Part 1: Evidence based research on Prophylactic antibiotic timing and SSIs incidences
Background
According to the national statistics, there are about 5% reports of surgical site infection (SSI) in all surgical processes every year. The study indicates that SSIs accounts about 2% of the mortality; and increases healthcare cost by 10 to 20%. Additionally, it has also been found that it increases hospital stays and increases the medical care costs (Shepard et al., 2013). Evidence based research indicates that about 60% of the SSIs are preventable if there the government implements quality based standards which should be implemented in the inpatient surgery. Therefore, the federal government should explore SSIs epidemiology, clinical consequences and the risk factors involved. This will help in establishing guidelines on the effective strategies such as hand hygiene, sustaining normothermia. This article explores the evidenced based practice that proper timing of prophylactic antibiotics could reduce the incidences of surgical site infection (Rafique, 2012).
Research indicates that SSIs are the second most challenge facing the public health. According to National Nosocomial Infection System, SSIs are infections that arise after operative procedures, within one month after the procedures. The efforts to lower the incidences of SSIs are not new concept. The efforts can be traced to the 19th Century with Lister who pioneered the use of antiseptic incidence in patients in the orthopedic ward. The issue of SSIs is not new in this health care facility (Teija-Kaisa, Eija, Marja, & Outi, 2012). For instance, about of 2% of patients undergoing surgical process in this health care facility reports SSIs. This causes about 5% readmission rates and 3% increase hospitalization days. In fact, it have been found that patients who present SSIs are 5 folds likely to be readmitted, with 60%of them being more likely stay in the ICU, and are two folds likely to pass away as compared to those who have no infection. The financial burden of the disease cannot be overlooked (Regimbeau et al., 2014; Hopper et al., 2015).
Purpose of the study
This study proposes that administering of prophylaxis antibiotics one hour before surgical procedures will lower the SSIs incidences. The study aims at establishing the most effective and best timing for the administration of the prophylactic antibiotic during the surgical procedures. This is because there is limited research on the adherence to the proposed Surgical Care Improvement guidelines; this has failed to prove that timely administration of prophylactic antibiotic reduces the incidence rates of SSIs (Alberta Health Services, 2014).
Evidence based practice
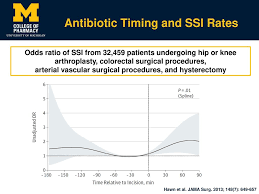
The issue of SSIs and its challenges is global. For instance, A retrospective study conducted using the Veterans affairs data on antibiotic administration timing on patient who were undergoing surgical procedures in the orthopedic, vascular, colorectal, and gynecologic procedures from 2005 to 2009 indicates that timing rate influenced the rate SSIs. Another study was conducted on 1922 patients who were primary care of hip arthroplasty in about 11 hospitals (Center for Healthcare Related Infection Surveillance and Prevention and Tuberculosis Control, 2012). The hip arthroplasty have been associated high morbidity due to their difficultness to study using the controlled trials. Additionally, the study indicated that the infection rate is generally low and would therefore not indicate significant outcomes. However, several other studies have indicates a proportional relationship indicating a U curve, with the lowest infection rate being recorded when the prophylactic antibiotic was administered about half an hour before incisions were made; and rates increased as time before the administration increased. Current US guidelines recommends that the prophylactic should be administered at least 60 to 120 min of incision (Fry, 2013).
Several other studies have demonstrated a good penetration of the tissue as well as excellent concentration of the antibiotics in the tissue when the administration of the antibiotic is done close incision time (Bowler, Welsby, Hogarth, & Towers, 2013).
The current clinical guideline on antimicrobial prophylaxis was developed by Burke. The guideline resulted from an investigation on the rate of inflammatory response on the surgical incision. The analysis found that the prophylactic antibiotic prophylactic process was most effective if the antibiotic was administered within 1 hour before the incision process. The analysis concluded that the bacteria were the most susceptible to the antibiotics, and their susceptibility was determined by the antibiotic timing as well as selection. Another retrospective study conducted by Classen and colleagues on 3000 patients who were undergoing surgical procedure indicated that patients received antibiotic one hour before the surgical process reported the lowest rates of SSIs (Anderson, 2014).
Study conducted by Merollini and colleagues using structured interviews on general practitioners, the nurses and physicians in the orthopedic department recommended the use of antibiotics within 30min to 1 hour before incision (Diamond, M. (2008). Other systematic review study, which used key words such as SSIs, orthopedic as well as prevention; indicated most studies reported that patients who received antibiotic prophylaxis would reduce the SSI rates to 1-3% in comparison to 4% without 8% with the control group. Based from this research study, one can therefore suggest that the most effective period to administer prophylaxis antibiotic is within one hour before the healthcare provider initiates the incision process because it reduces the risk of SSIs effectively (Center for Healthcare Related Infection Surveillance and Prevention and Tuberculosis Control, 2012).
Solution description
The proposed is that the healthcare providers in the surgical department will be encouraged to administer prophylactic antibiotic within one hour before the surgical process begins. This is because it will lead to reduction of the microorganism burden by three folds. Additionally, due to the increased residual effects associated with prophylactic antibiotic, the solution proposed will be consistent improved quality of life for patients, and reduced cost of care (Pearse et al., 2014).
However, just like many organization, this strategy could face numerous barriers from the healthcare providers. This is particularly so because the healthcare providers are not willing to change their routine pattern because they feel that they have been applying the same strategy for a long period of time, and would therefore hesitate to adopt the new developments/ change. To start with, the healthcare professionals in the surgical department tend to have low priority of the administration process (Fonseca, C. (2012).
This is attributable to the fact that they the anesthesiologists are more concerned in ensuring that the environment is safe, the right equipment is sterilized and safe. The healthcare professionals are more concerned about healthcare conditions that affect the patient immediately, and tend to ignore the impacts of SSIs because they do not affect the patient immediately. Some of the professionals claim that the administration process is tedious and time consuming thus limiting the administration of medication on time. Additionally, the healthcare facility workflow could limit the proper timing of the antibiotics .In most of the healthcare centers; the insertion of IV is done by the nurses and is time consuming. The healthcare facility process of communication could affect the communication of the new an effective protocols (Jarral, McCormack, Ibrahim, & Shipolini, 2010).
Majority of the health care facility communicate to their staff verbally, this indicates the importance of effective process of exchanging information such as use of automated systems to communicate new systems and to reduce confusions of adminsterring antibiotics in time by the nurses. Lastly, the concept of role perception determines the rate of drug administration, resulting to confusion as each healthcare provider denies that it is his or her responsibility. This causes further delays in the administration of the prophylactic antibiotic (Erb et al., 2014).
Implementation strategies
The first implementation strategy will be to educate the healthcare professionals in the surgical department on the important of using shorter duration for the administration of prophylactic antibiotic. The advantages will be discussed first with by the head of the surgical department with the aim of describing the feasibility of the matter. Secondly, poster concerning the best antibiotic agent and the recommended prophylactic antibiotic administration time will be hung in all vicinities surrounding surgical operation room including the physician room, the scrub sinks, and the operation room. This education is aims at enlightening the healthcare providers at individual level to transform the healthcare provider’s attitudes, behavior, as well as beliefs (Samant & Ramugade, 2014)
The second step will be to establish a multidisciplinary protocol that will be used to influence the healthcare providers on the effective management of SSIs through teamwork and effective communication, which will specify the timing as well as the sequences necessary for the achievement of the responsibility. Lastly, the institutions will implement the antibiotic timing programs, which will involve the integration of systems that will reduce, curtail, and control the process of antibiotic administration program. This will include approaches to measure parameters such as the written orders, computerized support programs among others (Feilmeier, Dayton, Sedberry, & Reimer, 2014).
Expected outcomes
Research associates increased utility of quality care improvements where the management of guidelines is followed reduces variability and miscommunication, which is often associated with increased medication and diagnostic errors. In this context, a successful intervention is one, which will involve identification of a nurse leader to serve and the motivator and change champions. This will require a number of in service refresher course training, use of systems that reminds the nurses on the timing of administration of prophylactic antibiotic and one with specific bench marking of physician. The ultimate expectations of these actions is to improve patients quality of life through reduced rates of SSIs, reduced hospital stays and overall reduction of the healthcare costs (Johnson Et al., 2013).
Part B: Picot analysis
| Research Question: How effective is prophylactic antibiotic administration timing effective in the reduction of Surgical Sites Infections Incidences (SSIs)? | |||
| Type of patient/Problem | Intervention | Comparison intervention | Outcome |
| Patient in surgical Wards | Close administration of antibiotics (within one hour) before incision | Compared to delayed administration of antibiotics | Reduced incidences of SSIs
Reduced readmission rates Reduced mortality and reduced length of hospital stays |
| Key word:
Colorectal patients, orthopedic, hip arthroplasty patients Surgical site infection |
Key Word Prophylactic antibiotics,
Administration rate within one hour Antibiotic Surgical site infection |
Key Word:
Prophylactic antibiotics, Administration rate within one hour Health care quality |
Key Word:
Hospital stays Readmission rates SSIs mortality Practice guidelines |
Search History
Literature search was done in three main databases using the University online database. The database included CINAHL, Proquest, and EBSCOhost. The key word used to run the search included ; Colorectal patients, orthopedic, hip arthroplasty patients, Surgical site infection, Prophylactic antibiotics, Administration rate within one hour, Antibiotic, Surgical site infection, Prophylactic antibiotics, Administration rate within one hour, Health care quality, Hospital stays, Readmission rates, SSIs mortality, Practice guidelines
From these key words, approximately 534 articles were generated. The articles were narrowed down using filter methods such as publication year. The articles chose were supposed to from 2010, to avoid generating outdated information. From these, the articles were narrowed down to 235, and when Key words “SSIs” and “prophylactic antibiotics” were applied, the articles were narrowed down to 45 articles. Out of these articles, 17 articles were chosen to compile the work based on the relevance of the abstract and the year of the publication.
Example
Hooper, T.D., Hibbert P.D., Hannaford, N.A, Jackson, N., Hindmarsh, D.M., Gordon, D.L., Coiera, E.C., Runciman, W.B.(2015). Surgical site infection—a population-based study in Australian adults measuring the compliance with and correct timing of appropriate antibiotic prophylaxis. Anesthesia and intensive care 43 (4); 461- 469
P- The population being studied by this article is the Australian Adults who are undergoing operative procedures. The problem being investigated is the rate of SSIs to evaluate the infection rates with and without correct timing of prophylactic antibiotic administration
- The intervention suggested by this article is that proper timing of the administration of the prophylactic antibiotic reduces the incidences of SSIs considerably.
C- The study compares health outcomes of patients who experienced proper timing of the administration of the drugs with those who had delayed administration of the drug.
O- The outcome evaluated is the rate of adherence to proper timing, reduced health care costs and overall improve quality of life for patient.
T- Not applicable
Reference list.
Alberta Health Services. (2014). Best Practice Guideline for the Selection, Handling, Application, Use and Storage of Patient Skin Antiseptic Products for Invasive Procedures Outside of the Operating Room. Retrieved May 31, 2015 from http://www.albertahealthservices.ca/hp/if-hp-ipc-bpg-skin-antiseptic-products.pdf
Anderson, D. (2014). Prevention of Surgical Site Infection: Beyond SCIP. AORN Journal, 99(2), 315-319. doi:10.1016/j.aorn.2013.11.007
Bowler, P., Welsby, S., Hogarth, A., & Towers, V. (2013). Topical antimicrobial protection of postoperative surgical sites at risk of infection with Propionibacterium acnes: an in-vitro study. Journal Of Hospital Infection, 83(3), 232-237. doi:10.1016/j.jhin.2012.11.018
Center for Healthcare Related Infection Surveillance and Prevention and Tuberculosis Control. (2012). Guideline: Surgical Skin Disinfection. Queensland Government. Retrieved May 31, 2015 from http://www.health.qld.gov.au/chrisp/ic_guidelines/documents/Guideline_CHRISP_01.pdf
Diamond, M. (2008). Postsurgical Adhesions. Seminars In Reproductive Medicine, 26(04), 287-288. doi:10.1055/s-0028-1082386
Erb, S., Sidler, J., Elzi, L., Gurke, L., Battegay, M., Widmer, A., & Weisser, M. (2014). Surgical and Antimicrobial Treatment of Prosthetic Vascular Graft Infections at Different Surgical Sites: A Retrospective Study of Treatment Outcomes. Plos ONE, 9(11), e112947. doi:10.1371/journal.pone.0112947
Feilmeier, M., Dayton, P., Sedberry, S., & Reimer, R. (2014). Incidence of Surgical Site Infection in the Foot and Ankle with Early Exposure and Showering of Surgical Sites: A Prospective Observation. The Journal Of Foot And Ankle Surgery, 53(2), 173-175. doi:10.1053/j.jfas.2013.12.021
Fonseca, C. (2012). Nursing Care Indicators to Nursing Homes. Journal Of Nursing & Care, 01(03). doi:10.4172/2167-1168.1000107
Fry, D. (2013). Use of surgical-site infection rates to rank hospital performance across several types of surgery ( Br J Surg 2013; 100: 628-637). British Journal Of Surgery, 100(5), 637-637. doi:10.1002/bjs.9040
Jarral, O. A., McCormack, D. A., Ibrahim, S., & Shipolini, A. R. (2010). Should surgeons scrub with chlorhexidine or iodine prior to surgery? Oxford Journals, 12 (6), 1017-1021. doi: 10.1510/icvts.2010.259796
Johnson, A., Zywiel, M., Jones, L., Delanois, R., Stroh, D., & Mont, M. (2013). Reduced re-infection rates with postoperative oral antibiotics after two-stage revision hip arthroplasty. BMC Musculoskeletal Disorders, 14(1), 123. doi:10.1186/1471-2474-14-123
Pearse, R., Harrison, D., MacDonald, N., Gillies, M., Blunt, M., & Ackland, G. et al. (2014). Effect of a Perioperative, Cardiac Output–Guided Hemodynamic Therapy Algorithm on Outcomes Following Major Gastrointestinal Surgery. JAMA, 311(21), 2181. doi:10.1001/jama.2014.5305
Rafique, H. (2012). A retrospective case series study of a single centre’s experience of surgical site infection following purse-string closure versus linear closure of ileostomy sites. International Journal Of Surgery, 10(8), S26-S27. doi:10.1016/j.ijsu.2012.06.141
Regimbeau, J., Fuks, D., Pautrat, K., Mauvais, F., Haccart, V., & Msika, S. et al. (2014). Effect of Postoperative Antibiotic Administration on Postoperative Infection Following Cholecystectomy for Acute Calculous Cholecystitis. JAMA, 312(2), 145. doi:10.1001/jama.2014.7586
Samant, P., & Ramugade, S. (2014). Successful use of intravitreal and systemic colistin in treating multidrug resistant Pseudomonas aeruginosa post-operative endophthalmitis. Indian J Ophthalmol, 62(12), 1167. doi:10.4103/0301-4738.126991
Shepard, J., Ward, W., Milstone, A., Carlson, T., Frederick, J., Hadhazy, E., & Perl, T. (2013). Financial Impact of Surgical Site Infections on Hospitals. JAMA Surgery, 148(10), 907. doi:10.1001/jamasurg.2013.2246
Teija-Kaisa, A., Eija, M., Marja, S., & Outi, L. (2012). Risk factors for surgical site infection in breast surgery. J Clin Nurs, 22(7-8), 948-957. doi:10.1111/jocn.12009
We can write this or a similar paper for you! Simply fill the order form!




