Evidence Based Practice in Health Care
Aims of the Module
This aim of this module is to enhance students’ understanding of how evidence based practice has come to underpin how health care is delivered. It will explore a wide range of evidence and enhance the ability to acquire and evaluate evidence
- Indicative Module Content
- Advanced literature searching techniques
- Sources and hierarchical ranking of evidence and how these influence decision making
- Formulating clinical question, PICO
- Clinical guidelines
- Numerical concepts
- Assessment Brief
- Assessment and Reassessment detail and Guidance
Intended Learning Outcomes
- Demonstrate the skills of locating high quality evidence that is capable of enhancing decision making in your own sphere of practice
- Demonstrate how evidence can be manipulated and analyse specific examples of this from your own sphere of practice
- Discuss how clinical guidelines are developed and how they evolve by analysing specific examples from your own area of practice
Assignment Guidelines
The purpose of the assignments is to give you the opportunity to demonstrate that you have considered the learning outcomes (above) and that you can apply them to practice. Follow the guidelines below and you will meet the learning outcomes.
You will find a sample assignment in the Course Materials area of Blackboard, along with a video of the Module Leader discussing the assignments. These will give you an idea of the structure and content. If you are unsure of what is required of you contact the Module Leader to seek clarification.
Formative Assignment
In 2 parts. Maximum of 1000 words (+10%) in total, NOT including PICO worksheet if it is included as an Appendix.
This will be submitted through Turnitin and you will receive feedback from the tutor aimed at assisting you with the final summative assessment.
Part 1 (Approx 500 words)
Identify a specific area of interest in your own sphere of practice and design a PICO question that would assist you and others in finding evidence based material that would underpin the area chosen and answer your PICO question. The question itself should be justified by supporting evidence ñ i.e. you should demonstrate, citing appropriate source(s) that it has value to the area of practice chosen.
You should then detail the process of the literature search, including the terms / refining parameters used. You should aim to demonstrate how the search was initially cast wide to include all potentially relevant material, followed by how the focus of the search was narrowed.
The search should indicate a range of databases and terms used during the search, along with any filters employed (e.g. Boolean, wildcard truncation, date / language filters etc.), as well as any other skills that you have gained that you feel are relevant to undertaking a high quality search. If you have a large number of terms at each stage of the search an Appendix can be included / referred to in order to save word count, but you must ensure that the main discussion covers the key steps at each stage of the search. You should then conclude the search by giving citations to a couple of pieces of evidence located.
The objective is to demonstrate that you have acquired a range of search skills capable of producing a focused / manageable array of evidence. It is not necessary to answer the PICO question, nor to evaluate the evidence located ñ the marks / Learning Outcome relate to the quality of the search skills demonstrated.
Aim to support the discussion with appropriate citations which indicate that you are following a recognised search strategy.
Note that the area of practice to which the PICO question relates will form the basis for the clinical guideline section of the summative assignment ñ see question below. Construct your PICO question with this in mind (i.e. do not pick a very obscure topic which will not appear in any clinical guidelines).
Part 2 (Approx 500 words)
Access or construct a diagram or table of the hierarchy of evidence and include this in your assignment with appropriate title / citation. Discuss why evidence towards the top of the hierarchy is considered more reliable than that lower down the hierarchy. The focus should be on how design of trials can reduce bias and increase the reliability and validity of findings. Additional marks will be given for considering limitations of the different types of evidence / trial.
THIS SHOULD NOT MENTION THE PICO QUESTION, IT SHOULD MERELY DISCUSS THE RELIABILITY AND BIAS OF EVIDENCE.
Summative Assessment
3500 words including the material from the formative thread
This assignment is divided into 3 main sections which will give you the opportunity to meet the 3 learning outcomes of the module. Word counts for each section are approximate – but you must not exceed the overall word count by more than 10% (note penalties above).
The first part of the assignment relates to the work that you did in the formative thread above, and you have had the chance to work on this following the feedback that you received.
Where possible the focus should be on relating the material to your own area of practice, although you should try to remain objective throughout (i.e. focus on what the assignment will do, not what you will do).
You must adhere to University and (where relevant) professional body confidentiality policies.
Introduction – 200 words (approx.)
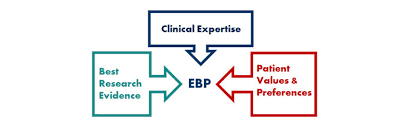
Give a brief account introducing the professional environment in which you work, along with a definition of evidence based practice and its relevance to practice.
There is no need to use first person ñ the entire assignment should be written objectively. For example, it might begin;
Working as a paramedic involves contact with patients
It is obvious that you are writing the assignment, and that this relates to your area of practice – therefore no need to state I work as a paramedic
PICO and the search for evidence- 1000 (Relates to LO 1)
Linked to / developed from the formative thread.
Briefly discuss the use of PICO as a tool for locating high quality evidence capable of supporting practice. This should include your PICO question, detailing how this helped shaped the literature search. Aim to include the PICO Worksheet which you can refer to in this section as a means of showing how your search skills have developed.
Summarise the hierarchy of evidence and how this is underpinned by trial designs that aim to reduce bias.
Practice Guidelines – 1000 (Relates to LO 3)
Note guidelines. A systematic review or randomised control trial are NOT examples of clinical guidelines. You international / national or local guidelines which make clinical recommendations.
Locate 2 clinical guidelines which are comparable in terms of their scope of practice (e.g. both on pain, or trauma management, or learning disabilities). Each should be compiled by a different body and do not need to be produced in the UK.
Using a recognised guideline analysis tool, compare and contrast the development of each guideline. Conclude by indicating which would be more suitable in practice, giving a clear rationale for your choice based on the analysis undertaken.
Most guidelines make the development process clear. You should aim to contrast the groups / individuals involved, the process that they used and how these contributed to producing the finished guideline. Aspects to consider include the range of expertise drawn upon, the involvement of external agencies and patient representation, the quality / breadth and currency of evidence upon which recommendations within the guidelines are made and the clarity of the recommendations themselves. Bear in mind that guidelines usually contain a number of recommendations; it is not necessary to examine each of these individually, the objective is to consider the guidelines as a whole.
In order to assist you in this process you MUST use a guideline evaluation tool, several of which are available in the Supplementary Materials section of Course Materials in Blackboard. The process of contrasting the guidelines should enable you to go on to provide a rationale for selecting one over the other.
Aim to sustain an objective approach throughout ñ no use of 1st person.
Additional marks will be awarded for taking a critical approach. For example, when considering members of the guideline development group, review dates or involvement of patients you might indicate (with supporting citation) what would be considered good practice in each case, or what these bring to the process of guideline development. Hepworth (20xx) indicates that taking a sustained critical approach in this way will result in a higher mark being awarded.
Manipulating the evidence ñ 1000 (Relates to LO 2)
Evidence can be manipulated in a variety of ways and for a variety of reasons. Critically discuss this statement.
This theme has run throughout the module and there are a number of approaches you might take here. You do not have to cover all examples of how evidence can be manipulated and would get better depth focusing on one – you might choose to focus on publication bias OR the effects of biased media reporting for example.
Whatever the focus, the assignment should aim to discuss the nature of the issue (what it is) and provide two or three examples of it having occurred, before concluding with a brief discussion of its implications.
The online activities provided you with a number of resources that would be of use in this regard.
To recap
- Define the type of manipulation to be discussed
- Give 2 or 3 detailed examples of it, indicating the manipulation which took place and any specific consequences / outcomes.
- Conclude with a brief discussion of the broader implications of manipulation of evidence ñ for providers and / or consumers of health care.
Conclusion / Opportunities – 300
Discuss how the use of the EBP skills acquired during the module might translate into opportunities for change in the stated area of practice. Be realistic here, and aim to include challenges inherent in this process – and keep the discussion objective.
Use the available word count
Evidence Based Practice in Health Care
Evidence based practiced (EBP) is used to determine the way clinical decisions are made by all health care professionals. It is widely used in paramedicine as practice based on prior research is more likely to result in a desired outcome for the patient (Youngblut and Brooten, 2001). This report will focus on how to locate evidence to substantiate the clinical decisions made by Paramedics on a day to day basis. Evidence can be in the form of randomised control trials (RCT’s), audits, knowledge from experienced professionals with extensive knowledge in the field and studies carried out by individual sponsors or pharmaceutical companies. It can also be taken from patient’s and service users experience.
EBP allows for para medicine to be more effective in enabling clinicians to make informed decisions surrounding a patient treatment and clinical interventions based on scientific research as oppose to practitioner’s individual opinions (Batt, 2014). This evidence needs to be of a high standard and kept up to date with the latest scientific evidence to influence a healthcare professional’s practice, so this report will also look at how evidence can be exploited to achieve a specific outcome. Clinical guidelines are documents which have been created to assist healthcare professionals in making decisions in their practice, this report will look closely at how information is gathered to be able to produce such documents. This will be done by scrutinizing two clinical guidelines used regularly in pre-hospital care. Within this report, evidence around the use of intravenous (IV) Paracetamol or IV Morphine in traumatic injuries will be evaluated for its authenticity.
In 2013/14, 21.7% of hospital attendances were for traumatic injuries (Baker, 2017). The ambulance service is often the first port of call for these patients to enable them to be conveyed to hospital in a timely manner, but also to have effective treatment prior to arriving with the notion of early intervention being vital. Paramedics dealing with musculoskeletal injuries would be looking to reduce the amount of pain a patient is in. To do this, they need to be able to determine the amount of pain they are in to begin with and utilise a variety of pain scales to do so. Three of the pain scales used in the pre-hospital setting include the Wong-Baker Faces pain rating, The Verbal Numerical Rating scale (VNRS) and The Abbey Pain Score (Lord, n.d.). The reason a variety of scales are used is due to the different patient groups that paramedics attend. These pain scores are documented prior to analgesia being administered as well as periodically afterwards. This is done to determine how effective the analgesics have been.
In the treatment of pain, there are a variety of pharmaceutical products that could be administered by a front-line paramedic, ranging from oral Paracetamol up to IV Morphine. In 1986, the WHO Pain Ladder was developed for patient’s dealing with pain secondary to cancer but since then, has widely been used for management of all types of pain. The pain ladder breaks the severity of pain down into three categories: mild, moderate and severe and indicates that for mild pain, non-opioids, such as aspirin or paracetamol, would be a starting point but for severe pain, opioid medication should be an early consideration (World Health Organisation, n.d.). NICE guidelines (2018) state that paracetamol is suitable for use in musculoskeletal pain and that opioid medications, such as morphine, should be used for moderate to severe pain. However, a study of paediatrics, conducted by Burke and Freedman (2018) notes that similar effects could be achieved for moderate to severe pain without the use of opioids.
To conduct a search into the evidence behind these findings, Heneghan & Badenoch (2006) recommend using a PICO question (Appendix 1.), which includes 4 key elements: population/patient, indicator/intervention, control, and outcomes (Aslam and Emmanuel, 2010). Is Paracetamol as effective as IV morphine in managing pain for patients with musculoskeletal (MSK) injuries? This question covers all aspects of the PICO question and formulates a very specific topic which has a vast array of prior evidence surrounding it. This subject area is pertinent to pre-hospital care as ambulance services in the UK often have resources that are manned by staff that are unable to administer controlled drugs, such as Morphine (England, 2016)…
We can write this or a similar paper for you! Simply fill the order form!




