Myocardial Infarction and a History of a Heart Attack Order Instructions: instructions and case scenario will be attached…..
an example will also be provided to help with writing the case study…
Myocardial Infarction and a History of a Heart Attack Sample Answer
Case study
Introduction
The case Describes Mr. Alphonse who has Myocardial infarction and a history of a heart attack. An ethical issue that comes out from the case is that the patient has offered a directive that he should not be resuscitated in the event he suffers a heart attack.
However, his close relatives have directed the staff to take notice of the advanced health directive. The health care providers have to make a decision on whether to follow the do not resuscitate order or to go by the relative’s decision to ignore the Advanced Health Directive. He is married and lives with his family and attends the church together. The legal issue in Mr. Alphonse case is the application of an Advanced Health Directive.
Facts
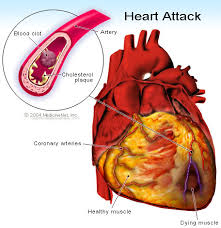
Myocardial infarction refers to the permanent damage of myocardial cells of the heart. It results from altered perfusion in a coronary artery due to occlusion by a clot (Berman et al., 2014). Coronary occlusion leads to reduced oxygen supply to the heart muscles. When a cell is deprived oxygen, ischemia results in injury and later death of cells. The condition manifests by chest pain which is not relieved by medication, shortness of breath, bradycardia, tachypnea and cold clammy skin (Berman et al., 2014). Diagnosis of the condition is made based on resenting symptoms, electrocardiography and laboratory tests. The patient describes the pain as a presenting symptom and a history of previous illness, a positive family history of a cardiac condition serves as a patient risk factor for the condition. An abnormal ECG and elevated cardiac enzymes confirm the diagnosis (Berman et al., 2014).
Myocardial infarction is managed pharmacologically using analgesics such as morphine, angiotensin converting enzymes, thrombolytic and nitrates. Myocardial infarction prognosis varies widely between individuals, presence or absence of risk factors present before the MI (Berman et al., 2014). Prognosis of Mr. Allophones was poor since he had survived the first attack therefore, he faced a substantial risk of further cardiovascular events such as stroke, angina, arrhythmias, heart failure recurrent and finally death.
Alternative management would have been emergent percutaneous coronary intervention. The intervention aims at promoting reperfusion of the area that had been deprived of oxygen (Berman et al., 2014). This form of management gets rid of underlying atherosclerosis lesion. Moreover, cardiac rehabilitation would have been done after the disappearance of the MI symptoms to target reduction of risk through education, individual and group support and physical activity (Berman et al., 2014). Social influence on the outcome of the condition includes; the family is responsible for participating in healthy living, encouraging the patients in attending cardiac rehabilitation programs and together with the patients they can help in developing plans to meet their specific needs.
Myocardial Infarction and a History of a Heart Attack and Ethical principles
Autonomy
This principle states that the client has the right to choose the course of treatment and act on that choice without interference from others. In this case, the patient is very much aware of his condition and has ordered that the other time he gets a cardiac arrest, he should not be resuscitated.
Myocardial Infarction and a History of a Heart Attack Beneficence
This principle stipulates that health care providers should promote actions that are beneficial to the patient without harm. Health care providers a have a responsibility of ensuring the wellbeing of the patient and get rid of anything that possesses danger on the health of the patient. According to this principle, the patient is well much aware of his condition and has made a decision about his will not to live by making an advanced health directive. This places himself at risk and therefore to honor this principle, nurses and other health care providers should prevent any harm, by ensuring the optimal health of the patient.
Nonmaleficence
This principle means the duty to cause harm which may take different forms; psychological, physical, social or spiritual harm which may either be actual or risk harm.in Mr. Alphonse’s case, risks which are posed is these possibility of developing a cardiac arrest together with pain. Therefore, the nurses must always be available to take care of any problem that may occur so as to ensure optimal health status by preventing any harm from the patient.
Justice
The principle of justice stipulates of the need for equal treatment and resource allocation for all individuals unless there is a justification for unequal treatment. Justice considers action from the point of view for the least fortunate in the society. As a result of equal and similar treatment of people, benefits and burdens are distributed equally. However, For Mr. Alphonse case, it has not been possible to balance the desires of the patient and the immediate relatives. Thus the nurse should make a decision on what seems to be best for the patient.
Myocardial Infarction and a History of a Heart Attack Ethical conflicts
Ethical conflicts results when there are conflicts between the two principles. Health care providers are caught in conflicts involving what ought to be done on the basis of one ethical principle and what not to be done on the basis of another principle (DeKeyser & Berkovitz , 2011).
Autonomy Vs. beneficence
Most often, there exists a conflict between the two ethical principles. Mr. Alphonse has made a decision that he does not want to be resuscitated next time he gets an attack. This is regard to the patient’s right to make his decision. However, the nurse is responsible for doing what benefits the patient and avoid the possibility of harm. Therefore, the nurse should resuscitate the patient should ensure the optimal health of the patient by resuscitated. However, there is a conflict of wanting to balance what the patient wants and the principle of doing well to the patient.
Myocardial Infarction and a History of a Heart Attack Autonomy Vs. non maleficence
Mr. Alphonse has been given all the information regarding the AHD and it is a desire that he is not resuscitated in the event he develops another heart attack. This respects the patient autonomy by allowing him to make a decision pertaining to his treatment. However, it goes against the principle of non-maleficence since
Myocardial Infarction and a History of a Heart Attack Considering Law
Sudden death from a cardiac arrest requires immediate resuscitation by a competent person. In health care settings, caregivers perform a CPR and other life saving measures unless the primary physician has written a do not resuscitate order in the client’s medical record. The physician’s order provides an exception to the universal standing order to resuscitate (Boddy et al., 2013). The principle of informed consent must be respected by the physician who writes the do not resuscitate order. A nurse has a responsibility to follow the client’s wishes relative to resuscitation. Furthermore, the caregivers must record the information in the client’s medical record.
An advance directive is a legal and formal document that provides instructions of care (Johnstone et al., 2015). Hence, individuals are accorded an opportunity to exercise their rights to make decisions in relation to their care in case they become incapable of active participation in health care decisions. These decisions are based on beliefs, values and attitudes regarding health, illness and death (Johnstone et al., 2015). Nurses have a responsibility of assisting their patients to make decisions about their care and protect their moral rights.
Furthermore, it enables them to communicate their wishes to their relatives, proxy and the primary care physician. The person signing the document must understand that the document is not only meant to be used when certain or all types of medical treatment are withheld but rather it allows for a detailed description of all health care preferences including full use of all available medical interventions (Boddy et al., 2013). The patient self-determination Act requires patient education about advanced directives at the time of hospital admission along with documentation of this education (Johnstone et al., 2015
Myocardial Infarction and a History of a Heart Attack Ethical decision
Ethical decision making requires one to thick critically what ought to be so as to provide justification of actions based on ethical principles. Therefore, health care providers must understand the bases which they make their decisions, it is important for them to note the decisions they make should not be based entirely on intuitions or emotions entirely (DeKeyser & Berkovitz , 2011). The Nursing and Midwifery Board of Australia 2015 states that the nurse has a right to make decisions for the patient by proper utilization of the decision making framework. For Mr. Alphonse case, I would respect his decision on the no resuscitate order. This is based on the ethical principle of autonomy. In addition, the law offers patients an opportunity to make advanced health directive provided correct information is provided.
An ethical foundation enables healthcare providers to be able to handle ethical conflicts in the best way.. In addition, it provides guidelines for healthcare providers with a framework for handling ethical dilemmas (DeKeyser & Berkovitz , 2011). With an ethical foundation that is based on ethical principles, health care providers can promote care to patients and families on end of life decisions.
Myocardial Infarction and a History of a Heart Attack Documentation
Documentation is an important aspect in health related profession. It is important for health professionals to note that the client’s medical record is a legal document. Through documentation, a healthcare provider will provide safe and sound care to the patient and thereafter it will help in the evaluation of the care provided to the patient. In the case of Mr. Alphonse, nurses must record all the information provided to the patient and the decision the patient makes thereafter. The information should be recorded in the patient medical record. In the event the patient dies, of which he did in this case, the medical document can be used in a court of law to prove that the patient had made a decision pertaining to his health.
The National and Midwifery Board of Australia (2010) considers documentation to be an important part of nursing practice an significant n the provision of quality care. Lack of proper documentation can lead to legal action on nurses and will impact on providing evidence in court for defense purposes and thus can be considered as malpractice. Thus, proper documentation can provide a powerful defense and protect nurses during legal accused or litigation process (Johnstone et al., 2015). Moreover, nursing and other health care providers should evaluate the care provided so as to help determine the effectiveness of the interventions carried out on a specific patient.
Myocardial Infarction and a History of a Heart Attack References
Berman, A., Snyder, S.J., Kozier, B., Erb, G., Levett-Jones T., Dwyer, T., Hales, M., Harvey, N., & Stanley, D. (2012). Kozier and erb’s fundamentals of nursing (2nd ed.). Vol 2, NSW: Pearson Sydney Australia.
Boddy, J., Chenoweth, L., McLennan, V., & Daly, M. (2013). It’s just too hard! Australian health care practitioner perspectives on barriers to advance care planning. Australian Journal of Primary Health, 19(1), 38-45.
DeKeyser Ganz, F., & Berkovitz, K. (2011). Surgical nurses’ perceptions of ethical dilemmas, moral distress and quality of care. Journal of Advanced Nursing, 68(7), 1516-1525.
Edvardsson, D., Watt, E., & Pearce, F. (2016). Patient experiences of caring and person‐centredness are associated with perceived nursing care quality. Journal of Advanced Nursing.
Hinkle, J. L. (2014). Brunner & Suddarth’s Textbook of Medical-surgical Nursing. K. H. Cheever, & J. L. Hinkle (Eds.).
Hoffmann, T. C., Montori, V. M., & Del Mar, C. (2014). The connection between evidence-based medicine and shared decision making. Jama, 312(13), 1295-1296.
Ingravallo, F., Gilmore, E., Vignatelli, L., Dormi, A., Carosielli, G., Lanni, L., & Taddi, P. (2014). Factors associated with nurse’s opinion and practices regarding information and consent. Nursing Ethics, 2(3), 259-313
Jackson, D., Hickman, L. D., Hutchinson, M., Andrew, S., Smith, J., Potgieter, I., … & Peters, K. (2014). Whistleblowing: an integrative literature review of data-based studies involving nurses. Contemporary nurse, 48(2), 240-252.
Jeffreys, M. R. (2015). Teaching cultural competence in nursing and health care: Inquiry, action, and innovation. Springer Publishing Company.
Johnstone , M. J., Hutchinson, A. M., Redley, B., & Rawson, H. (2015). Nursing Roles and Strategies in End-of-Life Decision Making Concerning Elderly Immigrants Admitted to Acute Care Hospitals An Australian Study. Journal of Transcultural Nursing,
Nursing and Midwifery Board of Australia. (2010). Nursing and national competency standards for Registered nurse.
O’Connell, J., Gardner, G., & Coyer, F. (2014). Beyond competencies: using a capability framework in developing practice standards for advanced practice nursing. Journal of advanced nursing, 70(12), 2728-2735.
Parahoo, K. (2014). Nursing research: principles, process and issues. Palgrave Macmillan.
Wilson, R. (2012). Legal, ethical and professional concepts with in the operating department. National Institute of Health, 22(3),81-5.




