Diagnosis and Management of Eye, Ear, Nose, and Throat Disorders
Order Instructions:
Diagnosis and Management of Eye, Ear, Nose, and Throat Disorders
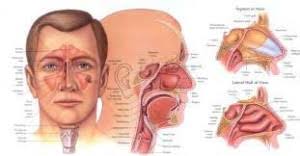
In clinical settings, eye, ear, nose, and throat (EENT) disorders account for the majority of pediatric visits. With the prevalence of these disorders, you must be familiar with their signs and symptoms as well as evidence-based practices for assessment and treatment. Although many pediatric patients present with common EENT disorders such as ear infections, allergies, and strep throat, some patients present with rare disorders requiring specialist care. In your role, making this distinction between when to treat and when to refer is essential. For this Discussion, examine the following case studies and consider potential diagnoses and management strategies.
Case Study
A mother presents with her 2-year-old child with complaints of ear pain and decreased sleep. Earlier this week, he had a runny nose and congestion with a mild cough that occurred mostly when lying down. His temperature is 100.7°F. You note the following physical findings: shotty anterior cervical adenopathy, mild nasal congestion, clear postnasal drainage, and lungs clear to auscultation. Ear examination reveals the following: right tympanic membrane is red, translucent, in a neutral position, with no pus or fluid noted; left tympanic membrane is full, reddish orange in appearance, and opaque with pus.
Assignment Paper:
Write two pages only on this discussion assignment (Let me give you a clue, the diagnosis of this case study is ACUTE OTITIS MEDIA)
1).write an explanation of the differential diagnosis for the patient in the case study
2). Explain which is the most likely diagnosis for the patient and why.
3) Include an explanation of unique characteristics of the disorder you identified as the primary diagnosis.
4). explain a treatment and management plan for the patient, including appropriate dosages for any recommended treatments.
5).Finally, explain strategies for educating parents on their child’s disorder and reducing any concerns/fears presented in the case study.
REFERENCES RECOMMENDED FOR THIS ASSIGNMENT (Please refer to the textbook)
• Burns, C. E., Dunn, A. M., Brady, M. A., Starr, N. B., & Blosser, C. G. (2013). Pediatric primary care (5th ed.). Philadelphia, PA: Elsevier.
Chapter 29, “Ear Disorders” (pp. 652–668)
this chapter reviews the structure and function of the ear and presents guidelines for the assessment and management of ear problems.
• American Academy of Pediatrics. (2004). Clinical practice guideline: Diagnosis and management of acute otitis media. Pediatrics, 113(5), 1451–1465. Retrieved from a Collage Library databases.
This article examines the diagnosis and management of uncomplicated acute otitis media in patients from 2 months to 12 years of age. It focuses on defining acute otitis media, pain management, assessment, and selection of appropriate antibacterial treatments.
• Chow , A.W., Benninger, M.S., Brook, I., Brozek, J.L., Goldstein, E.J.C., Hicks, L.A., Pankey, G.A., Seleznick, M., Volturo, G., Wald, E.R., & File Jr, T.M. (2012). IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clinical Infectious Diseases, 54(8), 72-112. Retrieved from a Collage Library databases.
• Shulman, S.T, Bisno, A.L., Clegg, H.W., Gerber, M.A., Kaplan, E.L., Lee ,G., Martin, J.M., & Van Beneden, C. (2012). Infectious Diseases Society of America. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clinical Infectious Diseases, 58(10), 86-102. Retrieved from a Collage Library databases.
SAMPLE ANSWER
Introduction
According to sources, AOM is a disorder that results from the malfunctions experienced in the Eustachian tube that results from colds, allergies, and bacterial infections. This can lead to the blockage of the inner linings with mucus. Out of this blockage, fluids build up and pile within the air-filled middle ear (Burns, Dunn, Brady, Starr, & Blosser, 2013). Germs and bacteria that enter these tubes breed in the fluids that are trapped in the ear thus leading to an ear infection known as the acute otitis media.
Acute Otitis Media (AOM) is a regular disease that involves the inflammation of the canals of the ear as a result of bacterial infections and pathogens that infect the ear. Some of the symptom present in this disease includes ear pains, decreased sleep, mild coughs, runny nose and congestion with an ear membrane that is red (Burns, et.al). This paper, therefore, seeks to study a patient presenting similar symptoms to AOM.
Case Analysis
The results of the diagnosis revealed that the child encountered some clinical signs and symptoms that included running nose and congestions that were accompanied by mild coughs. A high temperature of 100.7°F was also evident with other symptoms such as mild nasal congestion, and reddish appearance of the ear (Chow et.al).
The patient’s ear was in a neutral position and opaque with some sported pus. An infection was considered to be the main cause of the non-server unilateral AOM in the child. The diagnosis of this illness was found to be unilateral and non-severe because of the symptoms that were present in the child that required the use of antibiotics in the treatment. Severe cases of AOM would result in different symptoms.
The unique elements that could e noted in the child’s situation include the challenges she began encountering in feeding (Chow, et.al). The manifestation of ear tugging and lack of sleep are also factors that were unique in this child’s ailment. It is additionally necessary to remark that the child’s right tympanic ear membranes showed some redness in color with no fluids was also a unique factor that needed attention.
The Treatment and Management Plan of AOM
The management plan of the patient requires that, first of all, the child is relieved from pain. This requires that the child is prescribed antibiotics such as Amoxicillin for 30days. In an instance where the child is allergic to amoxicillin, she can be induced on an antibiotic with additional β-lactamase coverage (Shulman, Bisno, Clegg, Gerber, Kaplan, Lee, Martin, & Van, 2012). Amoxicillin, therefore, remains the best antibiotic for the child as recommended by a physician and according to an updated schedule. The child should also be introduced to an annual influenza conjugate vaccine. Breastfeeding should be exclusively encouraged
Educating Parents on Their Child’s Disorder
It is noteworthy that parents support their children to wash their hands with the aim of preventing flu and colds, a primary cause of otitis media (Dains, Baumann, & Scheibel.2012). The parents also have a role to play in ensuring that their children are not exposed to tobacco smoke and frequently attend day care for inspections. Parents should also be well informed of the use of the pacifiers and lastly giving the child and immunization to protect her from contracting AOM.
Conclusion
AOM is a disease that results from the malfunctions that are in most times experienced in the Eustachian tube from a cold, allergy, and a bacterial infection. In managing this ailment, a plan of the patient requires that, first of all, the child is relieved from pain. The use of amoxicillin remains the most efficient approach to managing this sickness in its mild state.
References
Burns, C. E., Dunn, A. M., Brady, M. A., Starr, N. B., & Blosser, C. G. (2013). Pediatric primary care (5th ed.). Philadelphia, PA: Elsevier. Chapter 29, “Ear Disorders” (pp. 652–668)
Chow, A.W., Benninger, M.S., Brook, I., Brozek, J.L., Goldstein, E.J.C., Hicks, L.A., Pankey, G.A., Seleznick, M., Volturo, G., Wald, E.R., & File Jr, T.M. (2012). IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clinical Infectious Diseases, 54(8), 72-112. Retrieved from a Collage Library databases.
Dains, J., Baumann, L., & P.Scheibel. (2012). Advanced health assessment and clinical diagnosis in primary care . St. Louis: MO: Mosby, Elsevier.
Shulman, S.T, Bisno, A.L., Clegg, H.W., Gerber, M.A., Kaplan, E.L., Lee, G., Martin, J.M., & Van Beneden, C. (2012). Infectious Diseases Society of America.58 (10), 86-102. Retrieved from a Collage Library database.
We can write this or a similar paper for you! Simply fill the order form!