Diagnosis and management of respiratory disorders; Asthma
Order Instructions:
Diagnosis and Management of Respiratory Disorders
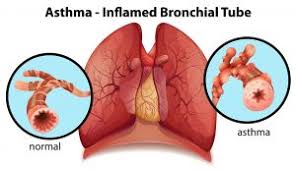
Respiratory disorders such as pneumonia and asthma are among the leading causes of hospitalization in pediatric patients (U.S. Department of Health and Human Services, 2011). With such severe implications associated with many respiratory disorders, advanced practice nurses must be able to quickly identify symptoms, diagnose patients, and recommend appropriate treatment. For this Discussion, consider potential diagnoses and treatments for the patients in the following the respiratory Disorders
Case Study
Brian is a 14-year-old known asthmatic with a 2-day history of worsening cough and shortness of breath. He reports using a short-acting beta agonist every 3 hours over the previous 24 hours. He has a long-acting inhaled corticosteroid, but the prescription ran out, and he forgot to get it refilled. He says he came today because he woke up at 2 a.m. coughing and couldn’t stop, thus preventing him from going back to sleep. Over-the-counter cough suppressants don’t help. He denies cigarette smoking, but his clothing smells like smoke. His respiratory rate is 18 and he has prolonged expiration and expiratory wheezes in all lung fields. There are no signs of dyspnea. All other exam findings are normal. (This asthma exacerbation in adolescent).
To prepare:
• Review Respiratory Disorders in the Burns et al. text.
• Review the provided case studies. Analyze the patient information.
• Consider a differential diagnosis for the patient in the case study. Think about the most likely diagnosis for the patient.
• Think about a treatment and management plan for the patient. Be sure to consider appropriate dosages for any recommended pharmacologic and/or non-pharmacologic treatments.
• Consider strategies for educating patients and families on the treatment and management of the respiratory disorder.
Assignment paper
Write 2 pages on
1) An explanation of these three differential diagnosis for the patient in the case study. (Asthma exacerbation, bronchiolitis, and laryngeal foreign body aspiration).
2) Explain which is the most likely diagnosis for the patient and why. (asthma exacerbation) Include an explanation of unique characteristics of this disorder you identified as the primary diagnosis.
3) Then, explain a treatment and management plan for the patient with asthmatic exacerbation including appropriate dosages for any recommended treatments.
4) Finally, explain strategies for educating patients and families on the treatment and management for asthma exacerbation.
REFERENCES RECOMMENDED FOR THIS ASSIGNMENT (Please refer to the textbook
• Burns, C. E., Dunn, A. M., Brady, M. A., Starr, N. B., & Blosser, C. G. (2013). Pediatric primary care (5th ed.). Philadelphia, PA: Elsevier.
o Chapter 31, “Respiratory Disorders” (pp. 708–738) and page 497-516 talks mostly on asthma and management)
this chapter covers the anatomy and physiology of the upper and lower respiratory tracts. It then explores assessment and management strategies for respiratory disorders including upper respiratory tract disorders, extrathoracic and intrathoracic airway disorders, and pectus deformity.
• National Heart, Lung, and Blood Institute. (2007). Expert panel report 3 (EPR3): Guidelines for the diagnosis and management of asthma. Retrieved from http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm
these reports provided by the National Heart, Lung, and Blood Institute present guidelines for the diagnosis and management of asthma in children from infancy through adolescence. The pathophysiology of asthma, measures of assessment and monitoring, control of environmental factors, and medication are also covered.
• Dexamethasone for Acute Asthma Exacerbations in Children: A Meta-analysis by Keeney, G.E., Gray, M.P., Morrison, A.K., Levas, M.N., Kessler, E.A., Hill, G.D., Gorelick, M.H., & Jackson J.L. in Pediatrics, 133(3): 493–499.
Copyright 2014 by American Academy of Pediatrics – Journals. Reprinted by permission of American Academy of Pediatrics – Journals via the Copyright Clearance Center.
• Mold, J.W., Fox, C., Wisniewski, A., Lipman, P.D., Krauss, M.R., Harris, D.R., Aspy, C., Cohen, R.A., Elward, K., Frame, P., Yawn, B.P., Solberg, L.I., & Gonin, R. Implementing asthma guidelines using practice facilitation and local learning collaboratives: a randomized controlled trial. Annals of family Medicine, 12(3), 233-240. Retrieved from the Walden Library databases.
SAMPLE ANSWER
Diagnosis and management of respiratory disorders
Asthma is the commonest respiratory disorder for kids. For Brian, the 14-year-old patient in the case study, three differential diagnoses for him are asthma exacerbation, bronchiolitis, and laryngeal foreign body aspiration. Asthma exacerbation: the major symptoms of this condition include coughing, a tight chest, shortness of breath, and wheezing (Keeney et al., 2014). Bronchiolitis: this is a common disease of the respiratory tract and is brought about by an infection which affects bronchioles – minuscule airways – which lead to the lungs. Bronchiolitis usually happens in the initial two years of life. Symptoms include being irritable, short pauses in breathing, persistent dry cough and rasping, wheezing, and vomiting after feeding (Burns et al., 2013). Laryngeal foreign body aspiration: kids who aspirate a foreign body at first usually present chocking and afterwards exhibit symptoms of respiratory syndrome. This condition is regarded as a differential diagnosis for asthma. Symptoms include gasping, coughing, chocking, and respiratory distress (Burns et al., 2013).
Of the three, asthma exacerbation is the most likely diagnosis for this patient. This is because the symptoms exhibited by the patient match with those of asthma exacerbations. In the case study, Brian has a 2-day history of worsening cough as well as shortness of breath. He woke up today with a persistent cough and he also has wheezes. All these symptoms – breathing faster, wheezing, persistent coughing, shortness of breath – are clear indications of asthma exacerbations (Mold et al., 2014). For the patient with asthmatic exacerbation, a treatment and management plan includes the following:
| Management of children aged above 12 years and adults | |||
| Medication | Dosage | Description | |
| Pharmacological intervention |
Short-acting beta 2 agonists |
· An inhaled, short-acting beta-2 agonist
· Use 2 or more canisters of beta2 agonists every months or 10-12 puffs daily |
Short-acting beta2 agonists usually work very fast and offer symptomatic relief (Keeney et al., 2014) |
|
Inhaled corticosteroids |
· Optimal dosages are 80 mg or less daily of methylprednisolone or 400 mg or less daily of hydrocortisone | Inhaled corticosteroids should be taken regularly where: symptoms disturb sleep every week, Beta2 agonists are being utilized over 2 times every week, and a kid has an asthma attack in the past 2 years necessitating systemic corticosteroids (Mold et al., 2014) | |
| Intravenous Salbutamol MDI with spacer | · 5 mg in 2 ml of normal saline every 20 minutes in the first hour | Patients who receive intravenous salbutamol have to be in a setting in which there is continuous cardiac monitoring (Burns et al., 2013) | |
| Non-pharmacological intervention | · Avoid exposure to cigarette/tobacco smoke
· Allergen immunotherapy should be considered for patients whose asthma symptoms are clearly connected to exposure to allergens (National Heart, Lung, and Blood Institute, 2007). |
||
It is worth mentioning that managing and treating asthma in children entails an appreciation of the existing treatment practice and a readiness to support and educate the asthmatic children and their close relatives in the longer-term. The strategies for educating patients and families on the treatment and management of asthma exacerbation entail providing smoking cessation advice to the child and caregivers/family members. This is important since passive or direct smoking decreases lung function and raises the need for rescue medication as well as long-term preventer treatment (Burns et al., 2013). Allergen avoidance should be included in the education: the patient may be allergic to pets and/or house dust mite. There could be pet allergy and it is sensible not to have a dog or a cat in the house since domestic pets may trigger an asthma attack. Physical and chemical techniques of house dust mite avoidance may trigger asthma exacerbations and should be avoided (Mold et al., 2014). Other trigger avoidance suggestions for the family include removal of soft toys from the bed, removal of carpets, washing of bed linen using high-temperature, improve ventilation, and using total bed-covering barrier systems. Education also includes encouraging adherence to asthma action plan to control asthma daily.
References
Burns, C. E., Dunn, A. M., Brady, M. A., Starr, N. B., & Blosser, C. G. (2013). Chapter 31, “Respiratory Disorders”. Pediatric primary care (5th ed.). Philadelphia, PA: Elsevier.
Keeney, G.E., Gray, M.P., Morrison, A.K., Levas, M.N., Kessler, E.A., Hill, G.D., Gorelick, M.H., & Jackson J.L. (2014). Dexamethasone for Acute Asthma Exacerbations in Children: A Meta-analysis. Pediatrics, 133(3): 493–499.
Mold, J.W., Fox, C., Wisniewski, A., Lipman, P.D., Krauss, M.R., Harris, D.R., Aspy, C., Cohen, R.A., Elward, K., Frame, P., Yawn, B.P., Solberg, L.I., & Gonin, R. (2014). Implementing asthma guidelines using practice facilitation and local learning collaboratives: a randomized controlled trial. Annals of family Medicine, 12(3), 233-240
National Heart, Lung, and Blood Institute. (2007). Expert panel report 3 (EPR3): Guidelines for the diagnosis and management of asthma. Retrieved fromhttp://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm
We can write this or a similar paper for you! Simply fill the order form!