Clinical reasoning
Clinical reasoning
Order Instructions:
APA REF. NOT OLDER THEN 5 YEARS.
ALL RESEARCH SHOULD BE VALID IN AUSTRALIA.
CASE STUDY IS HERE. PLEASE REFER TO FILES ATTACHED FOR MORE INFO
John Gray
28 years old
Severe depression following suicide attempt
?
Mr John Gray is a 28 year old single male admitted to the unit a week ago after an episode of intentional self-harm. John is the son of a grazier from a farming community north of Brisbane who is expected to take over the family farm. The farm has been severely affected by the longstanding drought conditions in the district. You are the nurse assigned to John’s care for the afternoon shift. On handover you were informed John did not get up for breakfast again, went to lunch reluctantly only because he was compelled to but ate almost nothing, and returned to his bed immediately afterwards. His routine morning observations were: Blood pressure 125/75, Temperature 36.3, Pulse 66, Respirations 18. John has a rope burn mark on his neck caused by the breaking of the rope with which he attempted to hang himself and some bruising and broken skin on his arms and legs from the subsequent fall but no serious physical injuries. The areas of broken skin were covered with a non-adherent dressing and tape. The occupational therapist reported John was still choosing not to take part in any activities, including small group games or one-on-one activity.
When you go to introduce yourself to John, you find him lying on his bed with the covers pulled up high. He appears reluctant to engage in conversation with you. When you address him to introduce yourself, he grunts and turns over to face the wall away from you.
Medications:
Venlafaxine 75 mg bd
Multivit i daily
Vit B co i daily
SAMPLE ANSWER
Introduction
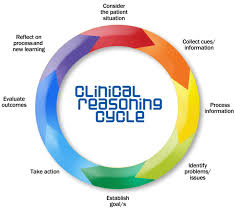
Clinical reasoning can also be termed as critical reasoning or clinical judgment (Kelton, 2014). It is the sourcing of clues about the patient’s symptoms in order to establish the cause of epidemiology rather than simply how to treat it. By looking at patient history, determining factors to the ailment and assessing response to previous medication, nursing staff can learn the patient’s immune system and propose better ways to treat the patient (Rugen et al, 2014). Clinical reasoning is a tactic in evident based practice. It comprises of; consideration for patient situation, collection of cues and data about the patient, processing these cues/information, identifying the problem or issue at hand, establishing treatment goals, taking action to administer treatment, evaluating the outcome of the treatment and reflecting on the outcome (Tsingos, Bosnic-Anticevich & Smith, 2014). This can be represented in the diagram below;
Considering the patient situation
Consideration for the situation of the patient involves aspects such as; listening to what the patient says, what their relatives say about the patient and assessing the condition. In some cases such as emergency nursing treatment where the cause for treatment is injury, little information is required to start the treatment (Jefford, 2012). There are indeed cases where the entire clinical reasoning process will not apply. However, clinical reasoning is very effective for chronic patient cases that include patients with cancer, arthritis, asthma, Leukemia and challenges such as kidney failure, diabetes and ulcers (Staveski, Leong, Graham & Roth, 2012).
Gathering Health Information
Health information can be gathered in many ways. The most popular of these ways is to check insurance records. The patient is to be made aware that such information is important for their treatment thus should be retrieved with their consent (Forbes & Watt, 2015). All records and files stored on chronic patients present a plethora of useful information that can really help nurses in offering care to the patients (Cockerham et al, 2011). For instance, a patient who has been catheterized needs to make it known before medical procedures are undertaken on them. Such knowledge may however not be present beforehand if the patient is brought in by non-relatives in a comatose /unconscious state of mind. Knowledge on past treatments helps avoid allergic reactions in current treatments as well (Andrew & Robb, 2011). It is thus important for nursing staff to be aware that they will require such information early hence begin looking for ways to source it.
Processing Information
With the entire information ready, there is need to process the information as it is. For instance, in the case of John, the patient in this case study, his history of causing self-harm cannot be easily diagnosed without having prior information on what the motivation for the harmful activities is. John’s friends and relatives can give the impression that he may have bipolar disorder, hyperactivity disorder, depression or an anxiety disorder. However, it is important to know if John has been using any drugs that may have either led to his disorders or aggravated the situation in the past. Currently, he is on Venlafaxine (anti-depressant medication), multivit (a dietary supplement) and vit B (Thiamine, Riboflavin and pantothenic acid). These medications indicate treatment for an eating disorder as well as depression.
Identifying the problem
The next step is to find out why Mr. John is depressed. It could be as a result of family, work or social issues. This information cannot be acquired from any other persons but the closest family members. Interviewing these family members would indicate reasons Mr. John may have been stressed to the point that he chose not to eat. In clinical reasoning, there is no assumption made. Every little detail about the person has to go into the preparation of the diagnosis (Bratt, 2013). Finding out the main reason for Mr. John’s stress can lead to the proper therapeutically-induced intervention for the patient. He may for instance need counseling more than he needs the medication he is on. Additionally, testing the patient’s vitals is very important in any diagnosis (Dariel, Raby, Ravaut & Rothan-Tondeur, 2013). From the vitals given; 125/75 mmHg, 36.30C, Pulse 66 and Respirations 18, he seems to be out of danger at the moment. Therapy thus seems to be the imminent treatment option.
Nursing Problems Based on Health Assessment
One of the key issues that I have identified from the provided case study is lack of patient cooperation. It is reported that Gray avoids engaging in conversations with health providers. This can result in ineffective delivery of patient care as they clinicians cannot properly tract the progress of Gray and provide quality care to him.
I am also concerned about Gray’s neck injuries and whether they could be linked to the depression that he is currently suffering from. Research by Cockerham et al., (2011) reports that severe neck or back pain can trigger can result in increased stress and depression. As a nurse, it is crucial to conduct a diagnosis aimed at determining whether the depression is lined to the pain.
The other nursing issue that perturbed me is Gray’s behavior of not eating or participating in recreational activities. Forbes & Watt (2015) enlighten that diet and activity are among the leading contributors of effective recovery from depression. Increasing the number of activities aids depressed patients such as Gray to cope with depression. Therefore, as a nurse I will encourage Gray to participate in events that he used to enjoy.
Goals for priority of Nursing care
Goals for priority of nursing care are based on various principles assigned within the clinical reasoning cycle. The most important goal is to ensure that all information acquired from interviewing John’s contacts is captured and recorded for future use. The next goal is to ensure that error omission is guaranteed by progressively seeking additional information to help in the diagnosis and treatment of the patient. Whether the information provided seems significant or not, it is vital to consider each new piece of information gained (Alfaro-LeFevre, 2012). It is also vital to ensure that the incorporation of pathophysiological knowledge into the treatment is balanced with the use of previous data and current information from significant sources.
Nursing Care for John
John is on the right track to recovery based on the medication given to him. However, the treatment of mental disorder and eating disorder is not sufficient. He needs to be under constant surveillance without making it seem like he is being monitored. He also needs to seek counseling. However, many patients often face denial and may not be willing to take this step. As a result, the primary nursing solution would be to talk to John about his actions and over time, get him to admit that he needs psychological help. By doing so, John can be fully assisted and on the road to recovery. The medication he is taking needs to continue, as long as he is not cleared of his psychological problem by a psychologist. In priority nursing care, it is important to incorporate professional advice from colleagues and supervisors (LeMone et al., 2015). This diagnosis thus needs to be discussed with other senior nursing officials to establish the degree of accuracy in the diagnosis.
Evaluating outcomes
The outcomes anticipated by the proposed nursing care for John include; admission of depression or mental problem, agreement to consult psychologist or the use of the hospital-appointed psychologist, being more open about his issues and restoration of his former life. John has to eventually continue being a father, husband and colleague to friends and family. He thus ought to begin treatment that will make him open up about the problems he faces. The importance of these strategies is that at the end of the day, John needs to be treated. The medication he is using works on him but it is apparent that he does not take it willingly. He needs to have an attitude change to accept medication before any medical intervention can work (Staveski, Leong, Graham & Roth, 2012).
Reflection
John’s case is not an isolated one. He seems to be struggling with depression-related problems. These problems are social in nature (Alfaro-LeFevre, 2012). There is need however to incorporate evidence-based practice in the treatment of John’s depression that has led to eating disorders, attempted suicide and self-inflicted injuries. Therapy seems to be the best option. However, before he begins the therapy, John needs to take his medication and lower stress levels. Once this has been done, he can then be treated and offered the necessary counseling to deal with his depression.
References
Alfaro-LeFevre, R. (2012). Applying nursing process: the foundation for clinical reasoning. Lippincott Williams & Wilkins.
Andrew, N., & Robb, Y. (2011). The duality of professional practice in nursing: Academics for the 21st century. Nurse Education Today, 31(5), 429-433.
Barker, J. (2013). Evidence-Based Practice for Nurses: SAGE Publications. Sage.
Bratt, M. M. (2013). Nurse residency program: Best practices for optimizing organizational success. Journal for nurses in professional development,29(3), 102-110.
Cockerham, J., Figueroa‐Altmann, A., Eyster, B., Ross, C., & Salamy, J. (2011, October). Supporting newly hired nurses: A program to increase knowledge and confidence while fostering relationships among the team. InNursing Forum (Vol. 46, No. 4, pp. 231-239). Blackwell Publishing Inc.
dit Dariel, O. J. P., Raby, T., Ravaut, F., & Rothan-Tondeur, M. (2013). Developing the Serious Games potential in nursing education. Nurse education today, 33(12), 1569-1575.
Forbes, H., & Watt, E. (2015). Jarvis’s Physical Examination and Health Assessment. Elsevier Health Sciences.
Jefford, E. (2012). Optimal midwifery decision-making during 2nd stage labour: the integration of clinical reasoning into midwifery practice.
Kelton, M. F. (2014). Clinical Coaching–An innovative role to improve marginal nursing students’ clinical practice. Nurse education in practice,14(6), 709-713.
LeMone, P., Burke, K., Dwyer, T., Levett-Jones, T., Moxham, L., & Reid-Searl, K. (2015). Medical-surgical nursing. Pearson Higher Education AU.
Levett-Jones, T., Hoffman, K., Dempsey, J., Jeong, S. Y.-S., Noble, D., Norton, C. A., . . . Hickey, N. (2010). The ‘five rights’ of clinical reasoning: An educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’ patients. Nurse Education Today, 30(6), 517-519.
Rugen, K. W., Watts, S. A., Janson, S. L., Angelo, L. A., Nash, M., Zapatka, S. A., … & Saxe, J. M. (2014). Veteran affairs centers of excellence in primary care education: transforming nurse practitioner education. Nursing outlook, 62(2), 78-88.
Schmidt, N. A., & Brown, J. M. (2014). Evidence-based practice for nurses. Jones & Bartlett Publishers.
Staveski, S., Leong, K., Graham, K., Pu, L., & Roth, S. (2012). Nursing mortality and morbidity and journal club cycles: paving the way for nursing autonomy, patient safety, and evidence-based practice. AACN advanced critical care, 23(2), 133-141.
Tsingos, C., Bosnic-Anticevich, S., & Smith, L. (2014). Reflective practice and its implications for pharmacy education. American journal of pharmaceutical education, 78(1).
We can write this or a similar paper for you! Simply fill the order form!