Weight Management For Obese Children Order Instructions: For this paper I will be sending the details via email. It is important that they writer note that it is a continuation of order # 113827 and the writer must closely follow the sample paper attached in the email, The writer will also continue the paper from where it ends on the first paper completed in the order # above.

The writer will start from Step 2: Locate the Best Evidence and most importantly the writer will have to respect all the headings and sub-headings as in the sample paper. The sources for completing the paper cannot be more than 5 years old since it is an evidence base paper, and must include DOI where necessary. It is important to remember that they title of the paper we are working on is “Lack of proper education on patient with type 2 diabetes” The writer must also include at least 8 new sources formatted in APA , adding to the previous reference list of the first part of the paper.
I will email the sample paper containing the entire paper, the first part and the secoound part that has to be completed this week. I will also send the first part that was completed some weeks ago so that the writer can continue on that same paper since it is a continues paper. But again it is important that he note that it is a continues paper meaning he must add the reference to the previous ones and properly format them while respecting all headings and sub-headings just as in the sample paper.
Weight Management For Obese Children Sample Answer
Weight Management For Overweight/Obese Children: Parents Take Charge (PTC)
Quality care can be defined as appropriately identifying, evaluating, diagnosing and treating patients. The term quality in healthcare is correlated to professional knowledge and desired health outcomes (Institute of Medicine, 2012). It is also defined as being closely associated with patient safety (Mitchell, 2008). Clinical excellence is the goal of providing quality care. The process for achieving clinical excellence includes patient-centered care.
The patient is the focus and includes their concerns regarding their illness, values, beliefs and support network. Making the patient an active participant in their health care results in informed decision-making by the patient. Autonomy, nonmalfeasance, beneficence, justice and fidelity are ethical principles that are addressed as definitions of providing quality care and achieving excellence in primary care. America Nurses Association, American League of Nursing, and Center for Applied and Professional Ethics are organizations that set guidelines for excellence (Stanley, 2011). Quality and excellence in a clinical site is achieved through appropriate, comprehensive and timely care.
Examples of methods of providing clinical excellence include providing evidence-based treatment, the timely manner in which patients are seen from when they sign in, the offer of generics versus brand-name medications, patient education, open dialogue with patients and referrals to specialist as needed. Ethical considerations taken in account are the patient’s autonomy. The patient is provided information for full understanding of their illness, evaluation, treatment and alternative treatments so that the capability for informed decision-making is established.
Guidelines for the prevention, identification, assessment and management of overweight and obesity in adults and children include how to assess whether people are overweight or obese; what should be done to help people lose weight; how to care for people who are at risk due to their weight and how to help people improve their diets and increase their physical activity (The National Institute for Health and Clinical Excellence NHS, 2012). The intention of this paper is to present an evidence-based project (EBP) proposal for childhood obesity. Included in this paper is assessing the need for change in practice, appropriate theoretical models and frameworks, statement of problem, intervention, goals, systematic review of current research and design. Assessing the need for change in practice consists of identifying stakeholders, collecting internal data about current practice, comparing external data with internal data, identifying the problem and linking the problem with interventions and outcomes (Larrabee, 2012).
Step 1: Assessing the Need for Change in Practice
Stakeholders
The first step for the model of evidenced-base change is assessing the need for change in practice. To Abstract
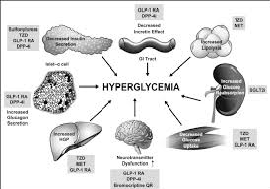
Diabetes is presently a popular chronic disease where the patient is required to make a wide array of self-management decisions daily as well as perform complicated care activities. Diabetes self-management education acts as the basis to assist the patients to navigate these activities and decisions. Kapoor and Kleinbart (2012) indicated that it greatly improves health outcomes. Diabetes education on self-management can be described as the process through which the skills, knowledge, and ability needed for the disease’s self-care is facilitated. As far as diabetes type 2 is concerned, patient education covers different aspects. Therefore, how effective the education is will greatly determine the extent to which the patient will engage in self-care. some of the aspects that patient education should cover includes the treatment options, disease process, causes, factors contributing to the disease, nutritional plan, exercise plan, knowledge about the medications that are prescribed, monitoring blood glucose, knowledge about the chronic and acute complications, individual approaches for promoting health, and the psychosocial issues (Mshunqane, Stewart & Rothberg, 2012). Regardless of how patient education is important, proper education still lacks, and there are a number of factors contributing to this. This paper aims at exploring the lack of proper education among diabetes type 2 patients.
Quality measures
Recently, NICE updated guidance on diabetes type 2 management. The National Collaborating Centre for Chronic Conditions developed the guidance. The then NICE guidelines are replaced and recommendations in some technology appraisals updated. The guidance will function as the only reference point for all care aspects. Worth noting, the guidance puts a lot of emphasis on patient education and complexities of management, lifestyle changes, as well as therapy side-effects have been made the priority. There is a recommendation that people suffering from diabetes type 2 should receive continuous education beginning from diagnosis, in addition to tailored dietary advice. The ADA’s (America Diabetes Association) position is that all diabetes patients should be provided with education and support from diagnosis and thereafter (Ruffin, 2016). The position statement is meant for the specific needs of people suffering from diabetes. This gives the indication that awareness among the patients is acknowledged as a very cardinal aspect for successful self-care.
Assessing the Need for Change in Practice
Stakeholders
The diabetes type 2 patients are the key stakeholders. These patients’ caregivers are also cardinal stakeholders since they mostly are concerned with caring for the patients. The entire healthcare team is a main stakeholder based on the fact that there are different aspects that should be monitored in patients on a regular basis (Green, 2014).
Barriers to Change
Some of the barriers that are likely to hinder change include the existing knowledge, fears and beliefs about the disease, accessibility to care, the influence of friends and peers, and health beliefs affect learning and consequently, the management behaviors. Therefore, it is worth pointing out that comprehending the expectations and needs of diabetes type 2 patients is cardinal in improving and initiating the education programs’ outcomes for effective self-care (Lee et al., 2013).
Facilitators to Change
Change can only be facilitated by making comprehensive explanations about the different aspects of the disease so that the patients can understand the impacts of failing to engage in the recommended practices. If patients have all the necessary details about the disease, then it would be easy for them to do away with the barriers that prevent proper information reception. For example, a patient who knows about the disease well is less likely to continue holding on health and spiritual beliefs that would only contribute to negative consequences (Garber, Gross & Slonim, 2010).
Internal Data
Many people present in healthcare institutions with the symptoms of diabetes type 2. An early diagnosis greatly ensures that complications are avoided and management done properly.
External Data
Everyone in Ontario ought to comprehend the disease’s seriousness since all are susceptible to it as well as the resulting health impacts. Diabetes type 2’s prevalence is alarmingly high. It is also expected to rise within the coming decade. In Ontario, more than 600,000 people suffer from the disease while many others are not yet aware that they have the disease. 4 out of 10 people suffering from the disease will develop long-term and debilitating complications. The disease is a known main cause of kidney disease, blindness, premature death, stroke, heart disease, and limb amputation among others.
Theoretical Model and Framework
The social learning theory that was crafted by Bandura is proper for exploring this issue at hand. It argues that people gain knowledge and skills after observing and imitating others, and through modeling. It also entails of aspects like memory, attention, and motivation. Learning occurs after people observe the attitudes as well as the behaviors of other people, in addition to the consequences of those attitudes and behaviors. Mostly, learning occurs through modeling and observation (Chijioke, Adamu & Makusidi, 2010). Therefore, if a given community continuously engages in activities aimed at managing and preventing diabetes type 2 which are encouraged by healthcare professionals, with lower disease rates, complications, and deaths as the effects, then all the communities around will imitate the particular community so as to realize similar impacts.
Problem
Regardless of the fact that various members in the community and from the healthcare team contribute in different ways to patient education, there is a great need for the providers as well as the practice settings to possess systematic referral processes and resources so that patients can receive education consistently. For example, the first education session might be offered by the healthcare professional while ongoing education sessions are offered by other practice personnel (Rosenstock & Owens, 2008). This can result to inconsistencies. Many times the programs that are designed fail to address the health beliefs, current knowledge, cultural needs, emotional concerns, physical limitations, financial status, family support, health literacy, medical history, and numeracy among other factors.
Problem Statement
There are numerous barriers that hinder effective patient education. Unless if those barriers are addressed, then even the most comprehensive education sessions will be useless (Stults-Kolehmainen & Sinha, 2014).
Possible Interventions
There is a great need for healthcare professionals to provide structured education to all diabetes type 2 patients and their care givers right from the diagnosis time. this should be accompanied by annual review and reinforcement. In addition, the practitioners ought to inform the caregivers and patients that the education is a cardinal component of diabetes care. The reviews should be conducted regularly based on need identification. Education should focus on all the good practice principles. In addition to this, the professionals should be keen at identifying the barriers that are likely to interfere with effective education reception or practice of all that was taught. The barriers should all be eliminated for effectiveness. Valencia and Florez (2014) noted that many patients anticipate diabetes education barriers. He, therefore, recommended that interventions at the multiple levels ought to address the socioeconomic and demographic diabetes education obstacles for effective self-management training (Zoepke & Green, 2012).
Critical Outcome Indicators
Definitely, following effective education among diabetes type 2 patients, numerous critical outcomes indicators would be evident. The patients would be able to make to make informed decisions about the treatment options that need, and understand more about the disease process. Moreover, they would be active in educating others about the causes and factors that contribute to the disease as a preventive measure. Moreover, following awareness creation on the proper diets, the patients would always be able to engage in appropriate nutritional and exercise plans, which would help prevent the related chronic diseases. The patients would also be able to engage actively and appropriately in monitoring blood glucose, taking right medications, taking the necessary measures to prevent the chronic and acute complications, promote health appropriately, and well as address the psychosocial issues (Augustyniak & Tadeusiewicz, 2009).
Goals and Purpose
Eliminating the barriers to diabetes education can ultimately improve patient experiences on education and care, improve populations and individuals’ health, as well as minimize diabetes- associated healthcare costs. In addition to eliminating the barriers, it is important to create an algorithm that defines what, how, and when the education should be offered to the patients.
Purpose Statement
Eliminating barriers to education and creating a proper algorithm can greatly promote effective education for better health.
References
Augustyniak, P., & Tadeusiewicz, R. (2009). Background 2.
Chijioke, A., Adamu, A. N., & Makusidi, A. M. (January 01, 2010). Mortality patterns among type 2 diabetes mellitus patients in Ilorin, Nigeria : original research. Journal of Endocrinology, Metabolism and Diabetes in South Africa, 15, 2, 79-82.
Garber, J. S., Gross, M., & Slonim, A. D. (2010). Avoiding common nursing errors. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.
Green, B. (June 06, 2014). Diabetes and diabetic foot ulcers : an often hidden problem : review. Sa Pharmacist’s Assistant, 14, 3, 23-26.
Kapoor, B., & Kleinbart, M. (April 01, 2012). Building an Integrated Patient Information System for a Healthcare Network. Journal of Cases on Information Technology (jcit), 14, 2, 27-41.
Lee YK, Ng CJ, Lee PY, Khoo EM, Abdullah KL, Low WY, Samad AA, Chen WS, & Lee, Yew Kong. (2013). What are the barriers faced by patients using insulin? A qualitative study of Malaysian health care professionals’ views. Dove Press.
Mshunqane, N., Stewart, A. V., & Rothberg, A. D. (January 01, 2012). Type 2 diabetes management : patient knowledge and health care team perceptions, South Africa : original research. African Primary Health Care and Family Medicine, 4, 1, 1-7.
Rosenstock, J., & Owens, D. (January 01, 2008). Treatment of Type 2 Using Insulin: When to Introduce?.
Ruffin, T. R. (January 01, 2016). Health Information Technology and Change.
Stults-Kolehmainen, M. A., & Sinha, R. (January 01, 2014). The Effects of Stress on Physical Activity and Exercise. Sports Medicine, 44, 1, 81-121.
Valencia, W. M., & Florez, H. (January 01, 2014). Pharmacological treatment of diabetes in older people. Diabetes, Obesity & Metabolism, 16, 12, 1192-203.
Zoepke, A., & Green, B. (January 01, 2012). Diabetes and diabetic foot ulcers : an often hidden problem : general review. Wound Healing Southern Africa, 5, 1, 19-22.
facilitate this, identification of stakeholders is needed. The target population is children, age 10-13 years and their families. Final decisions to change behaviors lies with the children, but parents have great influences over the young child’s meals, snacks and physical activities. Participating parents therefore, will be the change agent, adding them to the list of stakeholders. Parents make informed decisions regarding the health of their children with the help of a primary healthcare provider (Burns, Dunn, Brady, Starr, & Blosser, 2013). Primary healthcare providers or nurse practitioners (NPs) are stakeholders that will assist in facilitating and implementing change.
Barriers to Change
Barriers for children’s outcomes include their maturity level; ability to understand or commit to the program and their parents, if they are reluctant to participate. The primary barrier to change is participation of the parents. Physical activity and dietary behaviors will need modification in and out of the home. Without the participation of the parents the goal for long lasting results will not occur. Barriers for the parents include health literacy level; language, if the primary language is not English and attitudes towards modifying foods and physical activity. Another barrier is the participant’s adherences to the nutritional guidelines provided because diet plans do not include the cultural foods that the family consumes.
Facilitators to Change
Facilitators to change include support from their primary care provider or NP that the participants know and trust, educational classes that will be designed to meet their family’s cultural and specific needs and physical activities that can be done as a family that includes utilizing the workout facilities and pool in the local gym.
Internal Data
Internal data (date retrieved within Porterville Valley PromptCare Medical Center) provides overweight/obesity information that is defined by height, weight, body mass index (BMI), frequency of physical activity and anthropometric measurements of children in rural Tulare County, California.
External Data
External data (data retrieved outside of Porterville Valley PromptCare Medical Center) include the following (Ogden, Carroll, Kit & Flegal, 2012; California Center for Research on Women & Families, 2011):
a). Approximately 31.8 percent of children and adolescents aged 2—19 years are obese in the United States
b). Approximately 1 in 3 (33.2 percent) of children and adolescents age 6 to 19 years are considered to be overweight or obese in the United States
c). An estimated 30.5% of children and adolescents aged 10-17 years are presently overweight or obese in California
d). The total percentage of overweight and obesity from 1999 to 2009 rose from 34.0% to 37.6% for 9-11 year olds in California
e). For teens ages 12-17 years in California, African American youth had the highest percentage of overweight/obesity (39.9%), followed by Latinos (29.4%), Asian/other (18.0%) and white youth (12.0%)
Internal data presents an estimated 30% of the children seen in Porterville Valley PromptCare Medical Center are overweight or obese. When comparing Internal data and External data a change in practice is needed to prevent the incidence of childhood obesity from continuing to grow at an alarming rate.
Theoretical Model and Framework
Since this EBP proposal involves changes in physical activity and dietary behaviors understanding the effects of behavioral and social aspect of the child is necessary. With this in mind, the Transtheoretical Model will be discussed as an integral element in the design of PTC, an overweight/obese child intervention proposal.
Transtheoretical Model (TM)
The TM integrates clinical psychology and concepts to support a framework to understand the behavior and motivate behavioral change. The concepts of TM are decisional balance, processes of change, self-efficacy and temptation. The five stages of the transtheoretical model are the following: precontemplation (not intending to change), contemplation (considering a change), planning or preparation (actively planning change), action (actively engaging in a new behavior) and maintenance (taking steps to sustain change and resist temptation to relapse) (Kadowki, 2012).
Decisional balance occurs in each stage and involves the weighing of advantages and disadvantages towards changing behavior. The processes of change are the steps that facilitate understanding and behavioral change. Self-efficacy is essential and will vary depending on the TM stage. Temptation to revert back to previous stages will exist throughout the model. Support from the individual’s social network will provide the encouragement to continue within the program’s parameters.
Problem
A correlation between obesity and chronic diseases such as cardiovascular disease, diabetes mellitus and hypertension has been documented. Life expectancy for those who are obese is lower than those that maintain a normal Body Mass Index (BMI) (Centers for Disease Control and Prevention, 2011). Earlier death rates in adulthood have been linked to excess weight in the younger ages (American Heart Association, 2013). The prevalence of obesity has increased three-fold over the past few decades and is reported as a public health problem within the United States (Singh & Kogan, 2010). The cost of health care for obesity-related diseases (diabetes mellitus, hypertension, cardiovascular disease, etc) has skyrocketed and is predicted to continue to grow.
In the year 2000 an estimated $117 billion and $61 billion was spent both directly (medical costs) and indirectly (lost work time, disability, premature death and subsequent loss of income, etc) on overweight and obese individuals in the United States (Ward Smith, 2010). Chronic diseases linked to obesity were once seen mainly in adults, but are now becoming more and more prevalent in children. The National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP), Division of Adolescent and School Health (2010) reported “the prevalence of obesity among children aged 6 to 11 years increased from 6.5% in 1980 to 19.6% in 2008…and among adolescents aged 12 to 19 years increased from 5.0% to 18.1%” (NCCDPHP, Division of Adolescent and School Health, 2010). Health concerns for obese children are a reality that must be addressed since the effects of early obesity will impact their health for the rest of their lives.
Problem Statement
The problem addressed in this EBP proposal is the growing rate of childhood obesity and the negative effects on the child, parents, family and community.
Possible Interventions
Intervention of childhood obesity includes early identification and participating in health promotion activities such as eating healthier and becoming more physically active, as early as possible, to reduce the likelihood of chronic diseases and increase the health in those at risk. Wojcicki and Heyman (2010) stated “studies have shown that early interventions can potentially prevent the development of obesity in school-age children, along with associated health conditions” (Wojcicki & Heyman, 2010, p. 1457). Interventions of childhood obesity include promoting a balanced diet and increased frequency of physical activity. But, with the complexity behind childhood obesity, it requires other interventions as well. Vos, Wit, Pikl, Kruff and Houdijk (2011) stated their family-based cognitive behavioral multidisciplinary lifestyle treatment “aims to establish long-term weight reduction and stabilization, reduction of obesity related health consequences and improvement of self-image by change of lifestyle and learning cognitive behavioral techniques” (Vos et al., 2011).
Education and physical activity should be provided to the whole family in order to ensure successful lifestyle change to occur for the child. It is hoped that by encouraging whole family participation that a lasting positive outcome would result. Pender, Murdaugh and Parsons (2011) stated “the significant role the family plays in the development of both health-promotion and health-damaging behaviors, beginning at a very early age is well documented” (p. 243). Golley, Magarey, Baur, Steinbeck and Daniels (2007) stated “parenting-skills training combined with promoting a health family lifestyle may be an effective approach to weigh management in prepurbertal children, particularly boys” (p. 517).
Critical Outcome Indicators
Outcome indicators aim to achieve results that matter to the patient (Larrabee, 2012). Critical outcome indicators include improved BMI, improved laboratory measurements, improved health behavior, improved dietary patterns and increased frequency of physical activity.
Goals and Purpose
The health goal is to improve outcomes of obese children living in rural Tulare County, California. Quality goals are to improve access to diagnostics, early treatment and continuity of care with the use of evidence-based practices that include family participation. Quality measures include the participant’s understanding of the nature of obesity, treatment, the negative impact of obesity on lifestyle and overall health. These aspects will be measured through documentation of BMI status, weight classification, percent of physical activity and nutritional counseling.
Purpose Statement
The purpose of the EBP proposal is to promote health and well being in overweight/obese children and their whole family through participation in a nine-week multi-component, family-based community intervention program.
The writer will start from this point this week as the fisrt part was completed some 4 weeks ago.
Step 2: Locate the Best Evidence
Diabetes, hypertension and other co-morbid conditions associated with obesity and morbid obesity that were once conditions identified in adults only, is now increasing in obese children. The prevalence of obesity has more than doubled in the past 25 years in children aged 6 to 11 and has more than tripled for adolescents aged 12 to 19 (American College of Preventive Medicine, 2011). Interventions have been implemented to target the child’s risk factors, the parenting styles and family characteristics and environmental factors. The focus of this review was on parental involvement given the fact that parents are directly influential in how and what the child eats, the level of importance of physical activity and the limitation of video gaming and viewing of television programs in the home. Parental modeling of healthy behaviors is also an essential element in shaping the child’s lifestyle habits and behavior.
A systematic review of research consisting of parental involvement as an element of the intervention design for overweight/obese children was conducted. Interventions included changes in diet, increases in physical activity and behavior modification. The intention was to establish an intervention that produced the greatest possible outcome for the weight management of overweight or obese children through parental involvement.
Methods
Search Strategy
The following databases were examined for this systematic review: Medline, CINAHL, ERIC, Cochrane Central Register of Controlled Trials (CENTRAL), PSYCLinfo, Science Citation Index, and Social Science Citation Index, from 2005 to present. Reference lists from recent studies were also viewed to reinforce what was found during the formal search. Searches for references from studies and reviews were an element of data sources and were conducted for the following: children (6-17 years); parent participation/involvement and obesity, nutrition or physical activity-related behaviors (overweight, snacking, exercise and screen time). Inclusion criteria were primary language (English); at risk factors or behaviors associated with obesity; healthy children as participants and inclusion of at least one of the following at the child’s level: nutrition or physical activity-related behavioral or anthropometrical outcome. The retrieved data included intervention and characteristics of the study (context, outcome measures and process factors).
Step 3: Critically Analyze the Evidence
Four out of the eleven studies were non-RCT with either no treatment control; three alternate delivery formats; no treatment and non-participant controls; and usual care control (Graf et al., 2006, Lane-Tillerson, Davis, Killion & Baker 2005, Korsten-Reck, Kromeyer-Hauschild, Wolfarth, Dickhuth, Berg, 2005, Schwartz et al., 2007). All non-RCT studies produced positive outcomes, but the strengths of their effectives were varied. The studies that focused on providing educational and motivational sessions to the parents resulted in the most positive outcomes. The studies that focused on the children separately did produce positive outcomes, but were found to not be as effective.
The remaining seven studies were RCT with either usual care control, assessor-blinding, alternate sun protection intervention or waitlist control (Nemet et al., 2005, Patrick, et al., 2006, Gillis, Brauner, Granot, 2007, Gollye, Magarey, Baur, Steinbeck, & Daniels, 2007, Kalavainen, Korppi, Nuutinen, 2007, McCallum et al., 2007, Savoye et al., 2007). All the RCT studies resulted in positive outcomes with strong effectiveness. Five of the studies had measures that presented high effectiveness with the parent and child attending sessions for diet modification, physical activity and behavior modification together. One study in which the parent and child (5-9 years) received interventions separately still presented positive outcomes although it did not measure as high an effectiveness as when the parent and child were together. Another study with the parent and child receiving interventions separately, produced positive outcomes and was seen to measure high effectiveness, but this was indicated as resulting due to the greater age (11-15 years) than those in the other studies.
Addressing nutrition, physical activity, video game/television screening time, behavioral skills and parental involvement for change are seen effective in decreasing childhood obesity. Interventions that had the agent for change as the child only, child and parent and parent only, resulted in positive outcomes (Kalavainen, Korppi, & Nuutinen, 2007; McCallum et al., 2007; Savoye, et al., 2007; Schwartz et al., 2007).
A lack of consistency among the approaches to the methods and design of the studies was evident which made identification of the best multi-component program for childhood obesity undecided. The studies that had the agent of child presented lower measures for effectiveness except for older children (11-15 years). This group presented greater measures for effectiveness due to the level of maturity and understanding. The way in which parents are involved in childhood obesity treatment interventions varied, but all focused on their role in helping the child lose weight. When the parent was the agent for change it was most likely to present with higher measures of effectiveness.
Parenting styles and level of parenting skills affect the consistencies of interventions for childhood obesity. The parent’s levels of commitment to the program were noted as being an issue for the importance attached to diet, physical activity and video game/television screen time. A higher measure of effectiveness was noted for parents that attended session with their child than those that attended separately.
The variation in parental involvement in the reviewed trials indicate that parental involvement was effective in improving childhood obesity, but was ineffective in providing evidence of how much parental participation was needed to increase the likelihood of successful weight management. The age of the child was a factor in relations to parental involvement. Parents and children attending more sessions together were found to present greater effectiveness when the child was 7-13 years. It was found that parents attending sessions alone were more effectives for older children (11-15 years) and younger children (3-7 years). Obtaining effective treatment with parental involvement is important to identify for future treatments for childhood obesity.
Other limitations of the studies reviewed include inconsistent sample sizes, homogenous samples and the wide diversity in weight, BMI and anthropometric measurements. The complexities of childhood obesity require research that addresses all elements that affect the child. A growing body of evidence advocates a multidisciplinary, family-focused approach to childhood obesity management, but there is a need to explore interventions that allow for parental factors, such as how much time is appropriate for change to occur, commitment for change and understanding the needs for change in order for optimal effectiveness of the intervention to take place.
Feasibility, Benefits and Risks of Implementing the Practice Change
The feasibility of implementing the practice change in a primary cares setting is increased because routine visits by participants allow for screening and management of overweight children. The NP is able to use the established relationship with the patient and their family to present the practice change. The cost of staff training for identification of overweight/obese children, delivery of intervention and evaluation of intervention proposal will be minimal due to the primary care facility being already prepared to do so. The staff is already able to and is equipped to do the following:
- Record height and weight
- Calculate the participant’s BMI
- Record waist circumference
- Record biceps and triceps skinfold measurements
Potential Barriers
Parents themselves are a potential barrier due to their cultural background and belief system, commitment to the program, socioeconomic status and the need for the parents to change shopping behaviors and own eating behaviors. Identified economic barriers are time and dollar costs. Other barriers include child preference, difficulty with modifying habits, difficulty with monitoring child behavior and need for assistance from family members. The access to physical activity programs, availability of other foods to fast food, modification of video games/television time, dietary information that is cultural appropriate, making the child’s behavior changes gradually are other identified barriers.
Benefits
The impact of childhood obesity on the child’s physical health, emotional health and social health has been documented and has resulted in research for the most successful interventions that includes parental involvement. Benefits of making the practice change include increased consistency of evidence-based childhood obesity screening, early identification and education. Present research documents evidence that diet modification, consistent physical activity, behavior modification and goal setting are elements for weight management (Burns, Dunn, Brady, Starr, & Blosser, 2013). It was found that counseling on the child’s BMI status was linked to parental perception of the child weight status, which resulted in the parents being almost 10 times more likely to be motivated to make healthy lifestyle changes (Haemer, et al., 2011). The practice change will utilize the increased parental perception from the education sessions to assist the child in developing healthy lifestyle behaviors.
Risks
The risk of health conditions and disease caused by being overweight or obese include breast cancer, coronary heart disease, type II diabetes, sleep apnea, gallbladder disease, osteoarthritis, colon cancer, hypertension and stroke. Obesity is the second greatest cause of preventable death in the United States (Get America Fit Foundation, 2010) and has resulted in $14 billion in direct medical costs (National League of Cities, 2010). For the overweight/obese child the risks involve cardiovascular disease, the development of diabetes, bone and joint problems, sleep apnea, social and psychological problems and several types of cancer (Centers of Disease Control and Prevention, 2013). Risks involved for the healthcare facility in making the practice change include ineffectiveness, limited resources, time constraints, retention of participants and lack of evidence of best practice.
The effective interventions utilized counseling or education, handouts, motivation and support as behavioral strategies. But research on the amount and structure for parental involvement in weight management for overweight and obese children is limited and varied. Today’s overweight and obese children will most likely become tomorrow’s overweight and obese adults. The justification for making practice change to improve the clinical outcomes for childhood obesity through identified elements of parental involvement is essential for all stakeholders. Implications for design should include the cultural diversity and use of community resources.
References
American Academy of Child & Adolescent Psychiatry. (2011). Facts for families: Obesity in children
and teens. Retrieved from http://www.aacap.org/cs/root/fact_for_families/ obesity_in_children_and_teens
American College of Preventive Medicine. (2011). Adolescent obesity-Time for a
commitment to action: A resource from the American College of Preventive Medicine. Retrieved from www.acpm.org/resource/resmgr/…/ adolescentobesityclinicalref.pdf
American Heart Association. (2013). Overweight in children. Retrieved from
http://www.heart.org/HEARTORG/GettingHealthy/Overweight-in
Children_UCM_304054_Article.jsp
Burns, C. E., Dunn, A. M., Brady, M. A., Starr, N. B., & Blosser, C. G. (2013).
Pediatric primary care. (5th ed.). Philadelphia, PA: Elsevier Saunders.
California Healthline. (2013). Tulare County forum discusses obesity rates among
children in low-income families. Retrieved from http://www.californiahealthline.org/articles/2005/4/12/tulare-county-forum-discusses-obesity-rates-among-children-in-lowincome-families.aspx
Centers for Disease Control and Prevention. (2013). Childhood obesity facts: Health
effects of childhood obesity. Retrieved from http://www.cdc.gov/healthyyouth/ obesity/facts.htm
Centers for Disease Control and Prevention. (2011). Healthy weight – it’s not a diet it’s
a lifestyle! About BMI for adults. Retrieved from
http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html
Centers of Disease Control and Prevention. (2008). Steps to wellness: A guide to
implementing the 2008 physical activity guidelines for Americans in the workplace. Retrieved from http://www.cdc.gov/nccdpgp/dnpao/hwi/downloads/Steps2Wellness_BROCH14 _508_Tag508.pdf#page=70
Gajda, R. & Jewiss, J. (2004). Thinking about how to evaluate your program? These
strategies will get you started. Retrieved from http://pareonline.net/getvn.asp?v=9&n=8
Get America Fit Foundation. (2010). Obesity related statistics in America. Retrieved
from http://www.getamericafit.org/statistics-obesity-in-america.html
Gillis D, Brauner M, Granot E. A community-based behavior modification intervention
for childhood obesity. (2007). Journal of Pediatric Endocrinology, 20, 197–203.
Golan, M. & Weizman, A. Familial approach to the treatment of childhood obesity: Conceptual model.
(2001). Journal of Nutrition Education, 33(2), 102-107.
Gollye, R., Magarey, A., Baur, L., Steinbeck, K., & Daniels, L. (2007). Twelve-month
effectiveness of a parent-led, family-focused weight-management program for
prepubertal children: A randomized controlled trial. Pediatrics, 119(3), 517-
- doi: 10.1542/peds.2006-1746
Graf, C., Koch, B., Bjarnason-Wehrens, B., Sreeram, N., Brockmeier, K., Tokarski, W.,
Dordel, S., Predel, H. G. (2006). Who benefits from intervention in, as opposed to screening of, overweight and obese children? Cardiology in the Young, 16, 474–480.
Haemer, M., Cluett, S., Hassink, S. G., Liu, L., Mangarelli, C., Petereson, T., Pomietto,
M., Young, K. L., & Weill, B. Building capacity for childhood obesity prevention and treatment in the medical community: Call to action. Pediatrics (128), 2, S71 -S77
Institute of Medicine. (2012). Crossing the quality chasm: The IOM health care quality
initiative. Retrieved from http://ww.iom.edu/Global/News%20Announcements/Crossing-the-Quality-Chasm-The-IOM-Health-Care-Quality-Initiative.aspx
Kadowaki, L. (2012). The transtheoretical model and stages of change. Retrieved from
www.sfu.ca/uploads/…/GERO820_2012_Transtheortical_Mode.pdf
Kalavainen, M.P., Korppi, M.O., Nuutinen, O. M. (2007). Clinical efficacy of group-
based treatment for childhood obesity compared with routinely given individual counseling. International Journal of Obesity, 31,1500–1508.
Kaplan Higher Education. (n.d.). Fact sheet: The Kaplan University IRB at-a-glance.
Retrieved from http://www.kuctl.org/CTL_Develop/Courses_In_Progress/ PD523/doc_sharing/IRB_Fact_Sheet_6_25_2010.pdf
Korsten-Reck U., Kromeyer-Hauschild K., Wolfarth B, Dickhuth, H. H., Berg A. (2005).
Freiburg Intervention Trial for Obese Children (FITOC): results of a clinical observation study. International Journal of Obesity, 29, 356–361.
Lane-Tillerson C, Davis BL, Killion CM, Baker S. (2005). Evaluating nursing
outcomes: A mixed-methods approach. Journal of National Black Nurses Association, 16, 20–26.
Larrabee, J. H. (2012). Nurse to Nurse Evidence-Based Practice. ISBN: 0071493727
Publisher: McGraw-Hill
Mattessich, P. W. (2009). Evaluation of state nutrition, physical activity, and obesity
plans. Retrieved from http://www.cdc.gov/obesity/downloads/EvaluationofStateNPAOPlans.pdf
McCallum, Z., Wake, M., Gerner, B., Baur, L. A., Gibbons, K., Gold, L., Gunn, J.,
Harris, C., Naughton, G., Riess, C., Sanci, L., Sheehan, J., Ukoumunne, O. C., Waters, E. (2007). Outcome data from the LEAP (Live, Eat and Play) trial: a randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. International Journal of Obesity, 31, 630–636.
Mitchell, P. H. (2008). Chapter 1: Defining patient safety and quality care. Retrieved
from http://www.ncbi.nlm.nih.gov/books/NBK2681/
National Center for Chronic Disease Prevention and Health Promotion, Division of
Adolescent and School Health. (2010). Healthy youth: Childhood
obesity. Retrieved from http://www.cdc.gov/healthyyouth/obesity/
National Institutes of Health. (2005). Research involving vulnerable populations PHS
398 application instructions for completing the human subjects section for proposed research involving children. Retrieved from http://grants.nih.gov/grants/policy/hs/children4.htm
National League of Cities. (2010). Economic costs of obesity. Retrieved from
Nemet, D., Barkan, S., Epstein, Y., Friedland, O., Kowen, G., Eliakim, A. (2005).
Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics, 115, e443–e449.
Ogden, C. L., Carroll, M. D., Kit, B. K., & Flegal, D. M. (2012). Prevalence of obesity
and trends in body mass index among US children and adolescents, 1999-2010. Retrieved from http://jama.jamanetwork.com/article.aspx?articleid=1104932
Patrick, K., Calfas, K. J., Norman, G. J., Zabinski, M. F., Sallis, J. F., Rupp, J., Covin, J.,
Cella, J. (2006). Randomized controlled trial of a primary care and home-based intervention for physical activity and nutrition behaviors: PACE for adolescents. Archives of Pediatric Adolescent Medicine, 160, 128–136.
Pearson, K. (2011). Starter knowledge for childhood obesity: Tackling childhood obesity as a new
clinician. Retrieved from http://nurse-practitioners-and-physician-assistants.advanceweb.com/Features/Articles/Starter-Knowledge-for-Childhood-Obesity.aspx
Pender, N., Murdaugh, C., & Parson, M. A. (2011). Health promotion in nursing
practice. (6th ed.). Upper Saddle River, NJ: Pearson Educational, Inc.
Rao, G. (2008). Childhood obesity: Highlights of AMA expert committee recommendations. Retrieved
from http://www.aafp.org/afp/2008/0701/p56.html
Regents of the University of California. (2007). Adolescent Psychosocial Scales: Health and
environment survey. Retrieved from http://famprevmed.ucsd.edu/pacedocs/HES.pdf
Savoye, M., Shaw, M., Dziura, J., Tamborlane, W. V., Rose, P., Guandalini, C.,
Goldberg-Gell, R., Burgert, T. S., Cali, A. M., Weiss, R., & Caprio, S. (2007). Effects of a weight management program on body composition and metabolic parameters in overweight children: A randomized controlled trial. Journal of American Medical Association, 297, 2697–2704.
Schwartz, R. P., Hamre, R., Dietz, W. H., Wasserman, R. C., Slora, E. J., Myers, E. F.,
Sullivan, S., Rockett, H., Thoma, K. A., Dumitru, G., Resnicow, K. A. (2007). Office-based motivational interviewing to prevent childhood obesity: A feasibility study. Archives of Pediatrics & Adolescent Medicine, 161, 495–501.
Singh, G. K. & Kogan, M. D. (2010). Childhood obesity in the United States, 1976-
2008: Trends and current racial/ethnic, socioeconomic, and geographic disparities. Retrieved from www.hrsa.gov/healthit/images/mchb_obesity_pub.pdf
Stanley, J. M. (2011). Advanced practice nursing: Emphasizing common roles. (3rd
ed.). Philadelphia, PA: F. A. Davis Company.
The National Institute for Health and Clinical Excellence. (2012). Obesity, the
prevention, identification, assessment and management of overweight and obesity in adults and children. Retrieved from http://www.nice.org.uk/cg043
Vos, R. C., Wit, J. M., Pijl, H., Kruyff, C. C., & Houdijk, E. C. (2010). The effect of
family-based multidisciplinary cognitive behavioral treatment in children with
obesity: study protocol for a randomized controlled trail. Retrieved from http://www.trialsjournal.com/content/12/1/110
Ward-Smith, P. (2010). Obesity – America’s health crisis. Urologic Nursing, 30(4),
242-245. Retrieved from http://web.ebcohost.com.lib.kaplan.edu
Wojcicik, J., & Heyman, M. B. (2010). Let’s move-childhood obesity prevention from
pregnancy and infancy onward. New England Journal of Medicine, 362, 1457-1459. doi: 10.1056/NEJMp1001857
Appendix A
Golan and Weizman’s conceptual model: Familial approach to the treatment of childhood obesity, (Golan & Weizman, 2001).
Appendix B
Health & Environment Survey (Regents of the University of California, 2007).
Home & Environment Survey
Participant’s Name:________________________________________ Date:_________________________
Mother/ Father (Please Circle) Observation # ______________
Family Influences:
During a typical week, how often has a member of your household:
(Please check one number for each question only)
| Never | 1-2 days | 3-4 days | 5-6 days | Every day | |
| Watched your child participate in physical activity or play sports? | |||||
| Encouraged your child to do physical activities or play sports? | |||||
| Provided transportation so your child can do physical activity or play sports? | |||||
| Dona a physical activity or played sports with your child? | |||||
| Encouraged your child to eat fruits & vegetables? | |||||
| Discussed with your child how not eating fruits & vegetables can be unhealthy? | |||||
| Eaten fruits & vegetables with your child/ | |||||
| Encouraged your child to spend less time being sedentary (video/television screening time)? | |||||
| Discussed with your child how sedentary habits can be unhealthy? | |||||
| Helped your child to think of ways to reduce the time he or she spends on sedentary habits? | |||||
| Told your child that he or she is doing a good job reducing sedentary habits? | |||||
| Encouraged your child to eat lower fat foods? | |||||
| Eaten low fat foods with your child? | |||||
| Told your child that he or she is doing a good job eating low-fat foods? | |||||
| Encouraged your child to wear sunscreens? |
Food & Cooking
Are you the person who does most of the cooking in this child’s home?____Yes ____NO
If yes, please answer the following questions about cooking in your home.
If not, please answer the following questions to the best of your ability.
- When you prepare chicken, how often do you remove the skin?
- Never
- Occasionally
- Usually
- Always
- Never prepare chicken
- Which type of hamburger meat do you usually cook for your family?
- regular
- lean
- extra-lean
- never cook hamburger
- How often do you trim the fat off meat before you cook it?
- Never
- Occasionally
- Usually
- Always
- Never prepare meat
- What type of fat or oil do you use most often in cooking?
- lard
- meat fat (beef/pork/chicken drippings or chorizo)
- butter
- shortening
- margarine
- vegetable oil (olive, corn, canola, peanut oils, etc.)
g PAM or vegetable spray only
- never use fat or oil in cooking
- What type of mild o you usually serve?
- whole
- chocolate
- reduced fat (2%)
- low fat (1%)
- skim, nonfat, or powdered
- never use milk
- How often do you serve eggs?
- 5 or more times per week
- 3-4 times per week
- 1-2 times per week
- 1-3 times per month
- less than once per month
- never serve eggs
- When you buy or prepare refried beans, what type of fat are they usually made with?
- lard/butter
- bacon grease
- shortening
- vegetable oil
- PAM or vegetable spray
- none
- don’t know
- never serve refried beans
Neighborhood
About how long would it take to get from your home to the nearest businesses or facilities listed below if you walked to them? (Please check one box for each business or facility)
| 1-5 min | 6-10 min | 11-20 min | 21-30 min | 31+ min | |
| Convenience/small grocery store | |||||
| Supermarket | |||||
| Hardware Store | |||||
| Fruit/vegetable Market | |||||
| Clothing Store | |||||
| Post Office | |||||
| Library | |||||
| Elementary School | |||||
| Other School | |||||
| Your Job | |||||
| Bus Stop | |||||
| Park | |||||
| Recreation Center | |||||
| Gym or Fitness Facility |
Walking and Bicycling in your Neighborhood
Please check the answer that best applies to you and your neighborhood
| 1-5 min | 6-10 min | 11-20 min | 21-30 min | |
| Convenience/small grocery store | ||||
| Supermarket | ||||
| Hardware Store | ||||
| Fruit/vegetable Market | ||||
| Clothing Store | ||||
| Post Office | ||||
| Library | ||||
| Elementary School | ||||
| Other School | ||||
| Your Job | ||||
| Bus Stop | ||||
| Park | ||||
| Recreation Center | ||||
| Gym or Fitness Facility |
Neighborhood Surroundings
Please check the answer that best applies to you and your neighborhood
| Strongly Disagree | Somewhat Disagree | Somewhat Agree | Strongly Agree | |
| The streets in my neighborhood are hilly making it difficult to walk or bicycle in. | ||||
| There are many canyons/hillsides in my neighborhood that limit the number of routes to walk or bike. | ||||
| There are sidewalks in my neighborhood that are well maintained (no cracks etc…) | ||||
| There are bicycle or pedestrian trails in or near my neighborhood that are easily accessible. | ||||
| Sidewalks are separated from the road/traffic in my neighborhood by parked cars. | ||||
| There is a grass/dirt strip that separates the streets from the sidewalks in my neighborhood | ||||
| It is safe to rid a bike in or near my neighborhood | ||||
| There are trees along the streets in my neighborhood. | ||||
| There is tree cover or shade along the sidewalks in my neighborhood. | ||||
| There are many interesting things to look at while waling in my neighborhood. | ||||
| My neighborhood is generally free from litter. | ||||
| There are many attractive natural sights in my neighborhood such as views or landscaping. | ||||
| There are attractive buildings/homes in my neighborhood. |
Home Environment
Please indicate/check, which items you, have in your home, yard, apartment, complex or community
| Yes | No | |
| stationary aerobic equipment (bicycle, treadmill, etc…) | ||
| dog | ||
| trampoline for jogging in place | ||
| running shoes | ||
| swimming poll | ||
| weightlifting equipment | ||
| toning devices (physioballs, ankle weights) | ||
| aerobic workout videotapes | ||
| step aerobics, slide aerobics | ||
| skates (roller, in-line or ice) | ||
| sports equipments (balls, racquets) | ||
| canoe, row boat, kayak | ||
| skis (snow or water) |
Household Rules
Please check the answer that best applies to you and your family.
| Never | Sometimes | Usually | Always | |
| Do you limit the number of hours your child is allowed to watch TV? | ||||
| Do you limit the number of hours your child is allowed to play video/computer games? | ||||
| Is your child allowed to play outside without wearing sunscreen? | ||||
| Do you limit the amount of sweet snacks your child is allowed to eat? | ||||
| Do you limit the amount of soda your child is allowed to drink? | ||||
| Do you keep candy, cookies, or chips around the house that your child can easily get? | ||||
| Is your child allowed to play outside the home after dark? | ||||
| Is your child allowed to play in the park without an adult watching? | ||||
| How often does dinner in your child’s home include vegetables? | ||||
| How often does breakfast in your child’s home include fruit and/or 100% fruit juice? | ||||
| Are adults allowed to smoke cigarettes in your child’s home? |
Home Computer & Internet Use
Please indicate which items you have in your home, yard, apartment, complex or community
| Yes | No | |
| Do you have a computer in your home? | ||
| Do you have access to the Internet in your home? | ||
| If not to question 2, do you plan to get Internet access in your home in the next 6 months? |
Healthy Lifestyle Strategies
Rate how often in the past month you (or a family member) has done the following things to help your child lead a healthy lifestyle. A healthy lifestyle is a way of life that includes participating in physical activity, eating nutritious foods, and taking precautions against skin damage from the sun (Please check one box for each question)
| Never | Almost Never | Some-times | Often | Very Often | |
| Helped your child look for new information on healthy lifestyles in places like magazines, books, or on the Internet? | |||||
| Talked with your child about the benefits he or she will get from making healthy lifestyle changes? | |||||
| Talked with your child about how one’s surroundings (home and neighborhood) can affect healthy lifestyles? | |||||
| Encouraged your child to say positive things to himself or herself about making healthy lifestyle changes? | |||||
| Encouraged your child to think more about the benefits and less about the barriers to being healthy? | |||||
| Helped your child keep track of his/her progress making healthy lifestyle changes? | |||||
| Helped your child set short and long-term goals to make healthy lifestyle changes? | |||||
| Rewarded your child for making and sticking to healthy lifestyle changes? | |||||
| Helped your child find ways to get around the barriers to making healthy lifestyle changes? | |||||
| Put reminders around the home to help make and stick to healthy lifestyle changes? | |||||
| Reminded your child to not to get upset if sometimes he/she can not stick to a healthy lifestyle change goal? | |||||
| Encouraged your child to try different ways to make healthy lifestyle changes so that he or she will have more options to choose from? | |||||
| Encouraged your child to do things to make being healthy more enjoyable? |
Physical Activity
In answering the following questions,
- Vigorous physical activities refer to activities that take hard physical effort and make you breathe much harder than normal.
- Moderate activities refer to activities that take moderate physical effort and make you breathe somewhat harder than normal.
During the last 7 days, on how many days did you do vigorous physical activities like heavy lifting, digging, aerobics, running or fast bicycling? Think about only those physical activities that you did for at least 10 minutes at a time
_________________ days per week How much time in total did you usually spend on one of those days doing vigorous physical activities?
____________hours ___________minutes
During the last 7 days, on how many days did you do moderate physical activities like carrying light loads, or bicycling at a regular pace? Do not include walking? Think about only those physical activities that you did for at least 10 minutes at a time.
_________________ days per week How much time in total did you usually spend on one of those days doing moderate physical activities?
____________hours ___________minutes
During the last 7 days, on how many days did you walk for at least 10 minutes at a time? This includes walking at work and at home, walking to travel from place to place, and any other walking that you did solely for recreation, sport, exercise or leisure
_________________ days per week How much time in total did you usually spend walking on one of those days?
____________hours ___________minutes
The last question is about the time you spent sitting on weekdays while at work, at home, while doing course work and during leisure time. This includes time spent sitting at a des, visiting friends, reading, traveling on a bus or sitting or lying down to watch television.
During the last 7 days, how much time in total did you usually spend sitting on a weekday?
___________hours _________minutes
Appendix C
Fruits & Vegetables Stages (Regents of the University of California, 2007).
Fruits & Vegetables Stages
Mark the answer that is true for you.
| 0 Servings | 1 Servings | 2 Servings | 3 Servings | 4 Servings | 5 Servings | |
| How many servings of fruits and vegetables do you usually eat each day (a serving is 1/2 cup of cooked vegetables, 1 cup of salad, a piece of fruit, 3/4 cup of 100% fruit juice)? |
If you answered 0 to 4, do you think you will start eating 5 or more servings of fruits & vegetables a day in the next 6 months
_________No, and I do not intend to in the next six months
_________Yes, I intend to in the next six months
If you answered “5” or “6 or more” servings, have you been eating 5 or more servings of fruits and vegetables a day for more than 6 months?
_________Less than 6 months
_________6 months or more
Fruits & Vegetables Change Strategies
The following are activities, thoughts, and feelings people use to help them change their fruit & vegetable intake. Think of any similar experiences you may be having or have had in the past month. Then rate How Often you do each of the following:
| Never | Almost Never | Sometimes | Often | Many Times | |
| I set goals to eat at least five servings of fruits & vegetables a day | |||||
| I have a friend or family member who encourages me to eat more fruits & vegetables | |||||
| I say positive things to myself about eating fruits & vegetables | |||||
| I think about the benefits I will get from eating fruits & vegetables | |||||
| I reward myself for eating at least five servings of fruits & vegetables a day | |||||
| I look for information about ways to eat more fruits & vegetables | |||||
| I look for information about ways to eat more fruits & vegetables | |||||
| I keep track of the number of fruits & vegetables I eat |
Fruits & Vegetables Pros and Cons
The following statements are different beliefs about eating fruits & vegetables. Please rate How Important each statement is to your decision to eat 5 fruits & vegetables a day. Use the following scale:
| Not Important | Slightly Important | Moderate Important | Very Important | Extremely Important | |
| I would feel embarrassed if other kids see me eating fruits & vegetables | |||||
| I would have more energy if I ate fruits & vegetables | |||||
| I would be doing something good for my body if I ate fruits & vegetables | |||||
| I would need too much help from my parents to eat fruits & vegetables | |||||
| I would feel healthier if I ate fruits & vegetables | |||||
| My parents would be pleased if I ate fruits & vegetables | |||||
| I would rather eat sweets or high fat snacks than fruits & vegetables |
Fruits & Vegetables Confidence
There are many things that can get in the way of eating fruits & vegetables. Rate How Sure you are that you can do the following in each situation. Please answer All questions.
| I’m sure I can’t | I probably can’t | Neutral | I probably can | I’m sure I can | |
| Eat 5 servings of fruits & vegetables everyday | |||||
| Ask someone in your family to buy your favorite fruit or vegetable? | |||||
| Ask for fruits & vegetables with your lunch? | |||||
| Drink 100% fruit juice instead of fruit punch or soda? | |||||
| Eat fruits or vegetables for a snack instead of chips or candy? | |||||
| As someone in your family to include fruits or vegetables with dinner? | |||||
| Eat fruits & vegetables when eating out at a restaurant? |
Fruits & Vegetables Family Support
During a typical week, how often has a member of your household (your father, mother, brother, sister, grandparent or other relatives):
| Never | 1-2 days | 3-4 days | 5-6 days | Everyday | |
| Encouraged you to eat fruits & vegetables? | |||||
| Told you that you are doing a doog job with eating fruits & vegetables? | |||||
| Eaten fruits & vegetables with you? |
Dietary Fat Stage of Change
Do you consistently avoid eating high fat foods?
_____NO and I do NOT intend to in the next six months
_____NO, but I intend to in the next six months
_____NO, but I intend to in the next 30 days.
_____Yes, and I have been, but for LESS than 6 months
_____Yes, and I have been for more than 6 month
Appendix D
Screening Time
Screening Time spent for Television, Computer and Video Gaming
Mark the answer that is true for you.
| 0 hours | 1 hour | 2 hours | 3 hours | 4+ hours | |
| How many hours do you spend watching television during your free time Monday-Friday? | |||||
| How many hours do you spend playing video games during your free time Monday-Friday? | |||||
| How many hours do you spend playing or doing homework Monday-Friday on the computer? | |||||
| How many hours do you spend “surfing” the Internet or playing online games during Monday-Friday? |
Appendix E
NATIONAL INSTITUTES OF HEALTH
Diet History Questionnaire II
|
Today’s date:
| MONTH | DAY | YEAR | |
| Jan
Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec |
|___|___| | 2010
2011 2012 2013 2014 2015 2016 2017 2018 2019 2020
|
|
| 0 | 0 | ||
| 1 | 1 | ||
| 2 | 2 | ||
| 3 | 3 | ||
| 4 | |||
| 5 | |||
| 6 | |||
| 7 | |||
| 8 | |||
| 9 | |||
|
In what month were you born?
| Jan
Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec |
In what year were you born?
19 |___|___|
| 0 | 0 |
| 1 | 1 |
| 2 | 2 |
| 3 | 3 |
| 4 | 4 |
| 5 | 5 |
| 6 | 6 |
| 7 | 7 |
| 8 | 8 |
| 9 | 9 |
Are you male or female?
Male
Female
- Over the past month, how often did you drink carrot juice?
NEVER
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
- Over the past month, how often did you drink tomato juice or other vegetable juice?
(Please do not include carrot juice.)
NEVER
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
- Over the past month, how often did you drink orange juice or grapefruit juice?
NEVER (GO TO QUESTION 4)
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
|
3a. How often was the orange juice or grapefruit juice you drank calcium-fortified?
Almost never or never
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
- Over the past month, how often did you drink other 100% fruit juice or 100% fruit juice mixtures (such as apple, grape, pineapple, or others)?
NEVER (GO TO QUESTION 5)
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
4a. How often were the other 100% fruit juice or 100% fruit juice mixtures you drank calcium-fortified?
Almost never or never
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
- How often did you drink other fruit drinks (such as cranberry cocktail, Hi-C, lemonade, or Kool-Aid, diet or regular)?
NEVER (GO TO QUESTION 6)
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
5a. How often were your fruit drinks diet or sugar-free?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you drink milk as a beverage (NOT in coffee, NOT in cereal)? (Please do not include chocolate milk and hot chocolate.)
NEVER (GO TO QUESTION 7)
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
6a. What kind of milk did you usually drink?
Whole milk 2% fat milk 1 % fat milk Skim, nonfat, or ½% fat milk Soy milk Rice milk Other |
Over the past month…
- How often did you drink chocolate milk (including hot chocolate)?
NEVER (GO TO QUESTION 8)
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
7a. How often was the chocolate milk reduced- fat or fat-free?
Almost never or never
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
- How often did you drink meal replacement or high-protein beverages (such as Instant Breakfast, Ensure, Slimfast, Sustacal or others)?
NEVER
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
- How often did you drink soda or pop?
NEVER (GO TO QUESTION 10)
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
9a. How often were these sodas or pop diet or sugar-free?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
9b. How often were these sodas or pop caffeine-free?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you drink sports drinks (such as Propel, PowerAde, or Gatorade)?
NEVER
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
- How often did you drink energy drinks (such as Red Bull or Jolt)?
NEVER
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
- How often did you drink beer?
NEVER
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
Over the past month…
- How often did you drink water (including tap, bottled, and carbonated water)?
NO (GO TO QUESTION 14)
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
13a. How often was the water you drank tap water?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
13b. How often was the water you drank bottled, sweetened water (with low or no-calorie sweetener, including carbonated water)?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
13c. How often was the water you drank bottled, unsweetened water (including carbonated water)?
Almost never or never
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
- How often did you drink wine or wine coolers?
NEVER
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
- How often did you drink liquor or mixed drinks?
NEVER
| 1 time in past month | 1 time per day |
| 2–3 times in past month | 2–3 times per day |
| 1–2 times per week | 4–5 times per day |
| 3–4 times per week | 6 or more times per day |
| 5–6 times per week |
- How often did you eat oatmeal, grits, or other cooked cereal?
NEVER (GO TO QUESTION 17)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
16a. How often was butter or margarine added to your oatmeal, grits or other cooked cereal?
Almost never or never
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
- How often did you eat cold cereal?
NEVER (GO TO QUESTION 18)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
17a. How often was the cold cereal you ate Total Raisin Bran, Total Cereal, or Product 19?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
17b. How often was the cold cereal you ate All Bran, Fiber One, 100% Bran, or All-Bran Bran Buds?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
Over the past month…
17c. How often was the cold cereal you ate some other bran or fiber cereal (such as Cheerios, Shredded Wheat, Raisin Bran, Bran Flakes, Grape-Nuts, Granola, Wheaties, or Healthy Choice)?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
17d. How often was the cold cereal you ate any other type of cold cereal (such as Corn Flakes, Rice Krispies, Frosted Flakes, Special K, Froot Loops, Cap’n Crunch, or others)?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
17e. Was milk added to your cold cereal?
NO (GO TO QUESTION 18)
YES
17f. What kind of milk was usually added?
| Whole milk |
| 2% fat milk |
| 1% fat milk |
| Skim, nonfat, or ½% fat milk |
| Soy milk |
| Rice milk |
| Other |
- How often did you eat applesauce?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat apples?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat pears (fresh, canned, or frozen)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat bananas?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat dried fruit (such as prunes or raisins)? (Please do not include dried apricots.)
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat peaches, nectarines, or plums?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat grapes?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat cantaloupe?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat melon, other than cantaloupe (such as watermelon or honeydew)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat strawberries?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat oranges, tangerines, or clementines?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat grapefruit?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat pineapple?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat other kinds of fruit?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat COOKED greens (such as spinach, turnip, collard, mustard, chard, or kale)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat RAW greens (such as spinach, turnip, collard, mustard, chard, or kale)? (We will ask about lettuce later.)
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat coleslaw?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat sauerkraut or cabbage (other than coleslaw)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat carrots (fresh, canned, or frozen)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat string beans or green beans (fresh, canned, or frozen)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat peas (fresh, canned, or frozen)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat corn?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat broccoli (fresh or frozen)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat cauliflower or Brussels sprouts (fresh or frozen)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat asparagus (fresh or frozen)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat winter squash (such as pumpkin, butternut, or acorn)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat mixed vegetables?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat onions?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- Now think about all the cooked vegetables you ate in the past month and how they were prepared. How often were your vegetables COOKED WITH some sort of fat, including oil spray? (Please do not include potatoes.)
NEVER (GO TO QUESTION 47)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
46a. Which fats were usually added to your vegetables DURING COOKING? (Please do not include potatoes. Mark all that apply.)
| Margarine (including low-fat) | Corn oil
Canola or rapeseed oil |
| Butter (including low-fat) | Oil spray, such as Pam or others |
| Lard, fatback, or bacon fat | Other kinds of oils
None of the above |
| Olive oil |
- Now, thinking again about all the cooked vegetables you ate in the past month, how often was some sort of fat, sauce, or dressing added AFTER COOKING OR AT THE TABLE? (Please do not include potatoes.)
NEVER (GO TO QUESTION 48)
| 1 time in past month | 5–6 times per week |
| 2–3 times in past month | 1 time per day |
| 1-2 times per week | 2 times per day |
| 3-4 times per week | 3 or more times per day |
|
47a. Which fats, sauces, or dressings were usually added AFTER COOKING OR AT THE TABLE? (Please do not include potatoes. Mark all that apply.)
| Margarine (including low-fat) | Salad dressing
Cheese sauce |
| Butter (including low-fat) | White sauce
Other |
| Lard, fatback, or bacon fat |
- How often did you eat sweet peppers (green, red, or yellow)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat fresh tomatoes (including those in salads)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat lettuce salads (with or without other vegetables)?
NEVER (GO TO QUESTION 51)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
50a. How often did the lettuce salads you ate include dark green lettuce?
Almost never or never
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
- How often did you eat salad dressing (including low-fat) on salads?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat sweet potatoes or yams?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat French fries, home fries, hash browned potatoes, or tater tots?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat potato salad?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat baked, boiled, or mashed potatoes?
NEVER (GO TO QUESTION 56)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
55a. How often was sour cream (including low-fat) added to your potatoes, EITHER IN COOKING OR AT THE TABLE?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
55b. How often was margarine (including low-fat) added to your potatoes, EITHER IN COOKING OR AT THE TABLE?
Almost never or never About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
55c. How often was butter (including low-fat) added to your potatoes, EITHER IN COOKING OR AT THE TABLE?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
55d. How often was cheese or cheese sauce added to your potatoes, EITHER IN COOKING OR AT THE TABLE?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat salsa?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat catsup?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat stuffing, dressing, or dumplings?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat chili?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat Mexican foods (such as tacos, tostados, burritos, tamales, fajitas, enchiladas, quesadillas, and chimichangas)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat cooked dried beans (such as baked beans, pintos, kidney, blackeyed peas, lima, lentils, soybeans, or refried beans)? (Please do not include bean soups or chili.)
NEVER (GO TO QUESTION 62)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
61a. How often were the beans you ate refried beans, beans prepared with any type of fat, or with meat added?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat other kinds of vegetables?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat rice or other cooked grains (such as bulgur, cracked wheat, or millet)?
NEVER (GO TO QUESTION 64)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
|
63a. How often was butter, margarine, or oil added to your rice or other cooked grains IN COOKING OR AT THE TABLE?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat pancakes, waffles, or French toast?
NEVER (GO TO QUESTION 65)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
64a. How often was margarine (including low-fat) added to your pancakes, waffles, or French toast AFTER COOKING OR AT THE TABLE?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
64b. How often was butter (including low-fat) added to your pancakes, waffles, or French toast AFTER COOKING OR AT THE TABLE?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
64c. How often was syrup added to your pancakes, waffles, or French toast?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat lasagna, stuffed shells, stuffed manicotti, ravioli, or tortellini? (Please do not include spaghetti or other pasta.)
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat macaroni and cheese?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat pasta salad or macaroni salad?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- Other than the pastas listed in Questions 65, 66, and 67, how often did you eat pasta, spaghetti, or other noodles?
NEVER (GO TO QUESTION 69)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
68a. How often did you eat your pasta, spaghetti, or other noodles with tomato sauce or spaghetti sauce made WITH meat?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
68b. How often did you eat your pasta, spaghetti, or other noodles with tomato sauce or spaghetti sauce made WITHOUT meat?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
68c. How often did you eat your pasta, spaghetti, or other noodles with margarine, butter, oil, or cream sauce?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat bagels or English muffins?
NEVER (GO TO INTRODUCTION TO QUESTION 70)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
69a. How often were the bagels or English muffins you ate whole wheat?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
69b. How often was margarine (including low-fat) added to your bagels or English muffins?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
69c. How often was butter (including low-fat) added to your bagels or English muffins?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
69d. How often was cream cheese (including low-fat) spread on your bagels or English muffins?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
Over the past month…
The next questions ask about your intake of breads other than bagels or English muffins. First, we will ask about bread you ate as part of sandwiches only. Then we will ask about all other bread you ate.
- How often did you eat breads or rolls AS PART OF SANDWICHES (including burger and hot dog rolls)?
(Please do not include fast food sandwiches.)
NEVER (GO TO QUESTION 71)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
70a. How often were the breads or rolls that you used for your sandwiches white bread (including burger and hot dog rolls)?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
70b. How often was mayonnaise or mayonnaise-type dressing (including low-fat) added to the breads or rolls used for your sandwiches?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
70c. How often was margarine (including low-fat) added to the breads or rolls used for your sandwiches?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
70d. How often was butter (including low-fat) added to the breads or rolls used for your sandwiches?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat breads or dinner rolls, NOT AS PART OF SANDWICHES?
NEVER (GO TO QUESTION 72)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
71a. How often were the breads or rolls you ate white bread?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
71b. How often was margarine (including low-fat) added to your breads or rolls?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
71c. How often was butter (including low-fat) added to your breads or rolls?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
71d. How often was cream cheese (including low-fat) added to your breads or rolls?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat jam, jelly, or honey on bagels, muffins, bread, rolls, or crackers?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat peanut butter or other nut butter?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat roast beef or steak IN SANDWICHES?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat turkey or chicken COLD CUTS (such as loaf, luncheon meat, turkey ham, turkey salami, or turkey pastrami)? (We will ask about other turkey or chicken later.)
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat luncheon or deli-style ham? (We will ask about other ham later.)
NEVER (GO TO QUESTION 77)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
76a. How often was the luncheon or deli-style ham you ate light, low-fat, or fat-free?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
- How often did you eat other cold cuts or luncheon meats (such as bologna, salami, corned beef, pastrami, or others, including low-fat)? (Please do not include ham, turkey, or chicken cold cuts.)
NEVER (GO TO QUESTION 78)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
77a. How often were the other cold cuts or luncheon meats you ate light, low-fat, or fat-free? (Please do not include ham, turkey, or chicken cold cuts.)
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
- How often did you eat canned tuna (including in salads, sandwiches, or casseroles)?
NEVER (GO TO QUESTION 79)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
78a. How often was the canned tuna you ate water-packed?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
78b. How often was the canned tuna you ate prepared with mayonnaise or other dressing (including low-fat)?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
Over the past month…
- How often did you eat GROUND chicken or turkey? (We will ask about other chicken and turkey later.)
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat beef hamburgers or cheeseburgers from a FAST FOOD or OTHER RESTAURANT?
NEVER (GO TO QUESTION 81)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
80a. How often did you have cheeseburgers rather than hamburgers?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat beef hamburgers or cheeseburgers that were NOT FROM A FAST FOOD or OTHER RESTAURANT?
NEVER (GO TO QUESTION 82)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
|
81a. How often were these beef hamburgers or cheeseburgers made with lean ground beef?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat ground beef in mixtures (such as meatballs, casseroles, chili, or meatloaf)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat hot dogs or frankfurters? (Please do not include sausages or vegetarian hot dogs.)
NEVER (GO TO QUESTION 84)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
83a. How often were the hot dogs or frankfurters you ate light or low-fat?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat beef mixtures (such as beef stew, beef pot pie, beef and noodles, or beef and vegetables)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat roast beef or pot roast? (Please do not include roast beef or pot roast in sandwiches.)
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat steak (beef)?
(Please do not include steak in sandwiches)
NEVER (GO TO QUESTION 87)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
86a. How often was the steak you ate lean steak?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat pork or beef spareribs?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat roast turkey, turkey cutlets, or turkey nuggets (including in sandwiches)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat chicken mixtures (such as salads, sandwiches, casseroles, stews, or other mixtures)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat baked, broiled, roasted, stewed, or fried chicken (including nuggets)? (Please do not include chicken in mixtures.)
NEVER (GO TO QUESTION 91)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
90a. How often was the chicken you ate fried chicken (including deep fried) or chicken nuggets?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
90b. How often was the chicken you ate WHITE meat?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
90c. How often did you eat chicken WITH skin?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat baked ham or ham steak?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat pork (including chops, roasts, and in mixed dishes)? (Please do not include ham, ham steak, or sausage.)
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat gravy on meat, chicken, potatoes, rice, etc.?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat liver (all kinds) or liverwurst?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat bacon (including low-fat)?
NEVER (GO TO QUESTION 96)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
95a. How often was the bacon you ate light, low-fat, or lean?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
- How often did you eat sausage (including low-fat)?
NEVER (GO TO QUESTION 97)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
96a. How often was the sausage you ate light, low-fat, or lean?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat fried shellfish (such as crab, lobster, shrimp)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat shellfish (such as crab, lobster, shrimp) that was NOT FRIED?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat salmon, fresh tuna or trout?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat fish sticks or other fried fish (not including shellfish)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat other fish that was NOT FRIED (not including shellfish)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Now think about all the meat, poultry, and fish you ate in the past month and how they were prepared.
- How often was oil, butter, margarine, or other fat used to FRY, SAUTE, BASTE, OR MARINATE any meat, poultry, or fish you ate? (Please do not include deep frying.)
NEVER (GO TO QUESTION 103)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
102a. Which of the following fats were regularly used to prepare your meat, poultry, or fish? (Mark all that apply.)
| Margarine (including low-fat) | Corn oil
Canola or rapeseed oil |
| Butter (including low-fat) | Oil spray (such as Pam or others) |
| Lard, fatback, or bacon fat | Other kinds of oils
None of the above |
| Olive oil |
|
- How often did you eat tofu, soy burgers, or soy meat-substitutes?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat soups?
NO (GO TO QUESTION 105)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
104a. How often were the soups you ate bean soups?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
104b. How often were the soups you ate cream soups (including chowders)?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
104c. How often were the soups you ate tomato or vegetable soups?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
104d. How often were the soups you ate broth soups (including chicken) with or without noodles or rice?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
Over the past month…
- How often did you eat pizza?
NEVER (GO TO QUESTION 106)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
105a. How often did you eat pizza with pepperoni, sausage, or other meat?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat crackers?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat corn bread or corn muffins?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat biscuits?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat potato chips (including low-fat, fat-free, or low-salt)?
NEVER (GO TO QUESTION 110)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
109a. How often were the potato chips you ate fat-free? (Please do not include reduced-fat chips.)
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat corn chips or tortilla chips (including low-fat, fat-free, or low-salt)?
NEVER (GO TO QUESTION 111)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
110a. How often were the corn chips or tortilla chips you ate fat-free? (Please do not include reduced-fat chips.)
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat popcorn (including low-fat)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat pretzels?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat peanuts, walnuts, seeds, or other nuts?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat energy, high-protein, or breakfast bars (such as Power Bars, Balance, Clif, or others)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat yogurt (NOT including frozen yogurt)?
NEVER (GO TO QUESTION 116)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
115a. How often was the yogurt you ate low-fat or fat-free?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat cottage cheese (including low-fat)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat cheese (including low-fat; including on cheeseburgers or in sandwiches or subs)?
NEVER (GO TO QUESTION 118)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
|
117a. How often was the cheese you ate low-fat or fat-free?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat frozen yogurt, sorbet, or ices (including low-fat or fat-free)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat ice cream, ice cream bars, or sherbet (including low-fat or fat-free)?
NEVER (GO TO QUESTION 120)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
119a. How often was the ice cream you ate light, low-fat, or fat-free ice cream or sherbet?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat cake (including low-fat or fat-free)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat cookies or brownies (including low-fat or fat-free)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
- How often did you eat doughnuts, sweet rolls, Danish, or pop-tarts?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat sweet muffins or dessert breads (including low-fat or fat-free)?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat fruit crisp, cobbler, or strudel?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat pie?
NEVER (GO TO QUESTION 126)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
The next four questions ask about the kinds of pie you ate. Please read all four questions before answering.
125a. How often were the pies you ate fruit pie (such as apple, blueberry, others)?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
125b. How often were the pies you ate cream, pudding, custard, or meringue pie?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
125c. How often were the pies you ate pumpkin or sweet potato pie?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
125d. How often were the pies you ate pecan pie?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How often did you eat chocolate candy?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat other candy?
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
- How often did you eat eggs, egg whites, or egg substitutes (NOT counting eggs in baked goods and desserts)? (Please include eggs in salads, quiche, and soufflés.)
NEVER (GO TO QUESTION 129)
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
Over the past month…
128a. How often were the eggs you ate egg substitutes or egg whites only?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
128b. How often were the eggs you ate regular whole eggs?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
128c. How often were the eggs you ate cooked in oil, butter, or margarine?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
128d. How often were the eggs you ate part of egg salad?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
|
- How many cups of coffee, caffeinated or decaffeinated, did you drink (including coffee drinks such as Latte, Mocha, Frappuccino, etc.)?
NONE (GO TO QUESTION 130)
| Less than 1 cup in past | 5–6 cups per week |
| month | 1 cup per day |
| 1–3 cups in past month | 2–3 cups per day |
| 1 cup per week | 4–5 cups per day |
| 2–4 cups per week | 6 or more cups per day |
129a. How often was the coffee you drank decaffeinated?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- How many glasses, cans, or bottles of COLD or ICED tea, caffeinated or decaffeinated, did you drink?
NONE (GO TO QUESTION 131)
| Less than 1 glass, can or bottle in past month | 5–6 glasses, cans or bottles per week |
| 1–3 glasses, cans or bottles in past month | 1 glass, can or bottle per day |
| 1 glass, can or bottle per week | 2–3 glasses, cans or bottles per day |
| 2–4 glasses, cans or bottles per week | 4–5 glasses, cans or bottles per day |
| 6 or more glasses, cans or bottles per day |
130a. How often was the cold or iced tea you drank decaffeinated or herbal?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
130b. How often was the cold or iced tea you drank presweetened with either sugar or artificial sweeteners (such as Splenda, Equal, Sweet’N Low or others)?
| Almost never or never (GO TO QUESTION 131)
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
130c. What kind of sweetener was added to your presweetened cold or iced tea most of the time?
Sugar or honey
Artificial sweeteners (such as Splenda, Equal, Sweet’N Low or others)
|
Over the past month…
- How many cups of HOT tea, caffeinated or decaffeinated, did you drink?
NONE (GO TO QUESTION 132)
| Less than 1 cup in past | 5–6 cups per week |
| month | 1 cup per day |
| 1–3 cups in past month | 2–3 cups per day |
| 1 cup per week | 4–5 cups per day |
| 2–4 cups per week | 6 or more cups per day |
131a. How often was the hot tea you drank decaffeinated or herbal?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- Over the past month, did you add sugar, honey or other sweeteners to your tea or coffee (hot or iced)?
NO (GO TO QUESTION 133)
YES
132a. How often did you add sugar or honey to your coffee or tea (hot or iced)?
Almost never or never
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
|
132b. How often did you add artificial sweetener (such as Splenda, Equal, Sweet’N Low or others) to your coffee or tea?
Almost never or never (GO TO QUESTION 133)
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
132c. What kind of artificial sweetener did you usually use?
| Equal or aspartame |
| Sweet’N Low or saccharin |
| Splenda or sucralose |
| Herbal extracts or other kind |
- Over the past month, did you add whiteners (such as cream, milk, or non-dairy creamer) to your tea or coffee?
NO (GO TO QUESTION 134)
YES
133a. How often was non-dairy creamer added to your coffee or tea?
Almost never or never (GO TO QUESTION 133c)
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
133b. What kind of non-dairy creamer did you usually use?
| Regular powdered |
| Low-fat or fat-free powdered |
| Regular liquid |
| Low-fat or fat-free liquid |
133c. How often was cream or half and half added to your coffee or tea?
Almost never or never
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
133d. How often was milk added to your coffee or tea?
Almost never or never (GO TO QUESTION 134)
About ¼ of the time
About ½ of the time
About ¾ of the time
Almost always or always
133e. What kind of milk was usually added to your coffee or tea?
| Whole milk |
| 2% milk |
| 1% milk |
| Skim, nonfat, or ½% milk |
| Evaporated or condensed (canned) milk |
| Soy milk |
| Rice milk |
| Other |
|
Over the past month…
- How often was sugar or honey added to foods you ate? (Please do not include sugar in coffee, tea, other beverages, or baked goods.)
NEVER
| 1 time in past month | 3–4 times per week |
| 2–3 times in past month | 5–6 times per week |
| 1 time per week | 1 time per day |
| 2 times per week | 2 or more times per day |
The following questions are about the kinds of margarine, mayonnaise, sour cream, cream cheese, and salad dressing that you ate. If possible, please check the labels of these foods to help you answer.
- Over the past month, did you eat margarine?
NO (GO TO QUESTION 136)
YES
135a. How often was the margarine you ate light, low-fat, or fat-free (stick or tub)?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- Over the past month, did you eat butter?
NO (GO TO QUESTION 137)
YES
136a. How often was the butter you ate light or low-fat?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
- Over the past month, did you eat mayonnaise or mayonnaise-type dressing?
NO (GO TO QUESTION 138)
YES
137a. How often was the mayonnaise you ate light, low-fat or fat-free?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- Over the past month, did you eat sour cream?
NO (GO TO QUESTION 139)
YES
138a. How often was the sour cream you ate light, low-fat, or fat-free?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
- Over the past month, did you eat cream cheese?
NO (GO TO QUESTION 140)
YES
139a. How often was the cream cheese you ate light, low-fat, or fat-free?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
|
Over the past month…
- Over the past month, did you eat salad dressing?
NO (GO TO INTRODUCTION TO QUESTION 141)
YES
140a. How often was the salad dressing you ate light, low-fat or fat-free?
| Almost never or never
About ¼ of the time About ½ of the time About ¾ of the time Almost always or always |
The following two questions ask you to summarize your usual intake of vegetables and fruits. Please do not include salads, potatoes, or juices.
- Over the past month, how many servings of vegetables (not including salad or potatoes) did you eat per week or per day?
| Less than 1 per week | 2 per day |
| 1–2 per week | 3 per day |
| 3–4 per week | 4 per day |
| 5–6 per week | 5 or more per day |
| 1 per day |
|
|
- Over the past month, how many servings of fruit (not including juices) did you eat per week or per day?
| Less than 1 per week | 2 per day |
| 1–2 per week | 3 per day |
| 3–4 per week | 4 per day |
| 5–6 per week | 5 or more per day |
| 1 per day |
- Over the past month, which of the following foods did you eat AT LEAST THREE TIMES? (Mark all that apply.)
| Avocado, guacamole | Olives |
| Cheesecake | Oysters |
| Chocolate, fudge, or | Pickles or pickled |
| butterscotch toppings | vegetables or fruit |
| or syrups | Plantains |
| Chow mein noodles | Pork neck bones, hock, |
| Croissants | head, feet |
| Dried apricots | Pudding or custard |
| Egg rolls | Veal, venison, lamb |
| Granola bars | Whipped cream, regular |
| Hot peppers | Whipped cream, |
| Jell-O, gelatin
Mangoes |
substitute |
| Milkshakes or | |
| ice-cream sodas | NONE |
- For ALL of the past month, have you followed any type of vegetarian diet?
NO (GO TO INTRODUCTION TO QUESTION 145)
YES
144a. Which of the following foods did you TOTALLY EXCLUDE from your diet? (Mark all that apply.)
| Meat (beef, pork, lamb, etc.) |
| Poultry (chicken, turkey, duck) |
| Fish and seafood |
| Eggs |
| Dairy products (milk, cheese, etc.) |
|
The next questions are about your use of vitamin pills or other supplements.
- Over the past month, did you take any multivitamins, such as One-a-Day-, Theragran-, Centrum-, or Prenatal-type multivitamins (as pills, liquids, or packets)?
NO (GO TO INTRODUCTION TO QUESTION 147)
YES
- How often did you take One-a-day-, Theragran-, or Centrum-type multivitamins?
1–3 days in past month
1–3 days per week
4–6 days per week
Every day
146a. Did your multivitamin usually contain minerals (such as iron, zinc, etc.)?
| NO |
| YES |
| Don’t know |
146b. Over the past month, did you take any vitamins, minerals, or other herbal supplements other than your multivitamin?
NO
Thank you very much for completing this questionnaire! Because we want to be able to use all the information you have provided, we would greatly appreciate it if you would please take a moment to review each page making sure that you:
- Did not skip any pages and
- Crossed out the incorrect answer and circled the correct answer if you made any changes.
YES (GO TO INTRODUCTION TO QUESTION 147)
|
These last questions are about the vitamins, minerals, or herbal supplements you took that are NOT part of a One-a-day-, Theragran-, or Centrum-type of multivitamin.
Please include vitamins taken as part of an antioxidant supplement.
Over the past month…
- How often did you take Antacids such as Tums or Rolaids?
NEVER (GO TO QUESTION 148)
1–3 days in past month
1–3 days per week
4–6 days per week
Every day
147a. Was your antacid usually “extra strength”?
| NO |
| YES |
| Don’t know |
- How often did you take Calcium (with or without Vitamin D) (NOT as part of a multivitamin in Question 146 or antacid in Question 147)?
NEVER (GO TO QUESTION 149)
1–3 days in past month
1–3 days per week
4–6 days per week
Every day
148a. Did your Calcium usually contain Vitamin D?
| NO |
| YES |
| Don’t know |
148b. Did your Calcium usually contain Magnesium?
| NO |
| YES |
| Don’t know |
148c. Did your Calcium usually contain Zinc?
| NO |
| YES |
| Don’t know |
|
Over the past month…
- How often did you take Iron (NOT as part of a multivitamin in Question 146)?
NEVER
1–3 days in past month
1–3 days per week
4–6 days per week
Every day
- How often did you take Vitamin C (NOT as part of a multivitamin in Question 146)?
NEVER
1–3 days in past month
1–3 days per week
4–6 days per week
Every day
- How often did you take Vitamin E (NOT as part of a multivitamin in Question 146)?
NEVER
1–3 days in past month
1–3 days per week
4–6 days per week
Every day
The last two questions ask you about other supplements you took more than once per week.
- Please mark any of the following single supplements you took more than once per week (NOT as part of a multivitamin in Question 147):
| B-6
B-complex B-12 Beta-carotene Folic acid/folate Magnesium
|
Occu-vite/Eye health
Potassium Selenium Vitamin A Vitamin D Zinc |
- Please mark any of the following herbal, botanical, or other supplements you took more than once per week.
| Chondroitin
Coenzyme Q-10 Echinacea Energy supplements Fish oil/omega 3’s Flaxseed/oil Garlic Ginger Ginkgo biloba
|
Ginseng
Glucosamine/ chondroitin Peppermint Probiotics Saw palmetto Soy supplement Sports supplements St. John’s wort Other |
Thank you very much for completing this questionnaire! Because we want to be able to use all the information you have provided, we would greatly appreciate it if you would please take a moment to review each page making sure that you
Lack of proper education on patient with type 2 diabetes
Locating the Best Evidence
Often, diabetes type 2 patients lack proper education mainly because of the different barriers that they face as well as the receiving education that lacks a proper algorithm. Therefore, there is a great need for these measures to be acted upon so that the patients can realize more positive outcomes. Mshunqane, Stewart and Rothberg (2012) indicated that diabetes type 2 is associated with numerous complications, many of which can cause death if not managed appropriately. In addition to this, at the worldwide level, the disease is acknowledge as a main challenge that nags the policymakers each day. There is presently some staggering statistics of the increasing prevalence as well as the linked economic and health impact.
Further, the World Economic Forum, World Health Organization, as well as the United Nations recognize the challenge. All these bodies suggest for collective dedication to improve the life quality of the patients as well as prevent the disease. They are clear that the challenge is universal, urgent, and critical. There is also the acknowledgment that the disease is serious for two main reasons (Stults-Kolehmainen & Sinha, 2014). First is the health impacts linked to it which are more critical including increased likelihood for lower limb amputations, blindness, heart attacks, kidney failure, as well as stroke. Second, there are indirect and direct costs which are a major drain on the healthcare budgets as well as productivity.
The issue is very urgent considering that its prevalence is rising. Moreover, managing the complications associated with the disease is very costly, same as incorporating appropriate measures to ensure that the patients lead a high quality and independent life. The mentioned bodies also agree that proper education is one of the strategies through which the disease can be prevented and managed efficiently. However, there are a number of barriers that prevent this and the education algorithm normally used is inappropriate. Therefore, this systematic review will aim at finding information suggesting the appropriate algorithm as well as the common barriers as well as how they can be addressed.
Methods
Search strategy
Peer-reviewed academic journals will be sought from different databases, and these will be used to conduct the systematic review (Lee et al., 2013). The intention will be creating a proper algorithm on diabetes type 2 education, as well as identify some of the barriers to proper education and how they can be addressed. The databases to be used for the systematic review are CENTRAL, Social Science Citation Index, Science Citation Index, PSYCLinfo, Medline, ERIC, and CINAHL. The references to the articles that were selected were also evaluated for leads. Reading the reviews was necessary as it helped identify if the article was appropriate. In relation to the inclusion criteria, there was selection of articles that were not older than five years. Particularly, there was selection of those discussing the barriers to proper diabetes type 2 education and their solutions, and those discussing proper education standards (Kapoor & Kleinbart, 2012).
Critically Analyzing the Evidence and Synthesis
Proper education algorithm
Diabetes type 2 education preventive measures will be informed to all the people through local barazas. This would ensure that all people engage in appropriate lifestyles to prevent the disease. Cultural competent educators, and those with proper listening and communication skills will be used to offer the education so that no one can be left behind (Garber, Gross & Slonim, 2010). It will be necessary to educate the patients on all aspects of the disease including the causes, risk factors, predisposing factors, preventive strategies, available treatments, and management. In addition, awareness on how a patient can ensure self-care should be offered, same as the complications and the direct and indirect costs that a family can suffer because of the disease. Moreover, the educator should go into details when elaborating on the preventive measures including the diet and physical activity. The more the patients and all people know about the disease and how it is connected to other chronic conditions, the more efficiently they can engage in self-care (Green, 2014).
Barriers and addressing them
for patients to be able to receive the recommended diabetes type 2 education, they should really be concerned about their healthcare and ready to access or seek quality medical education. However, because of the ignorance some patient have, they prefer using over-the-counter medications or seeking traditional medicine men. They never seek the quality healthcare services because of their ignorance and low socioeconomic backgrounds. Therefore, even the use of preventive services among these patients is very minimal. To address this, the local authorities will be given a chance to mobilize people from their living areas, so that education can start at the grassroots level before even being offered at the healthcare institution (Zoepke & Green, 2012).
In addition, there are many elderly people suffering from the disease and with hearing, memory, and vision challenges. These will be offered the education in the presence of caregivers who can assist them around (Chijioke, Adamu &Makusidi, 2010).
Feasibility, Benefits, and Risks
Feasibility
The project of delivering proper education to the patients is feasible, especially if the most appropriate education is being delivered, with a consideration of the personal factors, and if the barriers that might hinder the education have been considered and measures to address these put in place. Healthcare providers would only need to offer patients attending the institution for medical care services the pamphlets containing all the necessary information. However, when dealing with diabetes type 2 patients, it would be necessary to find out first what they already know and later creating awareness while dispelling the misconceptions. This would be relatively cheap. It would also be necessary to explore other factors that affect individual patients so that advice can be offered (Rosenstock & Owens, 2008).
Barriers
After proper education is offered and the barriers to it addressed, some patients might still lack the funds to purchase even the affordable local foods. Considering that some patients might be elderly, there might be issues such as improper vision, hearing loss, and memory loss, which might influence practice of the education.
Benefits
Ensuring that the patients are receiving proper education and implementing it is essential in that it can go a long way in reducing the high prevalence of the disease, preventing complications, reducing the high costs needed to treat and manage the condition, as well as the losses related to loss of productivity and need for a higher quality of life (Ruffin, 2016).
Risks
Some of the anticipated risks include limited resources to ensure that adequate and proper education is being delivered to the patients (Valencia &Florez, 2014). In addition, there might be absence of cultural competence professionals to deal with patients from different backgrounds. In addition, tracking the patients at their homes to ensure that they are implementing the proper education appropriately can be difficult and costly.
References
Chijioke, A., Adamu, A. N., &Makusidi, A. M. (2010). Mortality patterns among type 2 diabetes mellitus patients in Ilorin, Nigeria : original research. Journal of Endocrinology, Metabolism and Diabetes in South Africa, 15, 2, 79-82.
Garber, J. S., Gross, M., & Slonim, A. D. (2010). Avoiding common nursing errors. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.
Green, B. (June 06, 2014). Diabetes and diabetic foot ulcers : an often hidden problem : review. Sa Pharmacist’s Assistant, 14, 3, 23-26.
Kapoor, B., & Kleinbart, M. (2012). Building an Integrated Patient Information System for a Healthcare Network. Journal of Cases on Information Technology (jcit), 14, 2, 27-41.
Lee YK, Ng CJ, Lee PY, Khoo EM, Abdullah KL, Low WY, Samad AA, Chen WS, & Lee, Yew Kong. (2013). What are the barriers faced by patients using insulin? A qualitative study of Malaysian health care professionals’ views. Dove Press.
Mshunqane, N., Stewart, A. V., & Rothberg, A. D. (January 01, 2012). Type 2 diabetes management : patient knowledge and health care team perceptions, South Africa : original research. African Primary Health Care and Family Medicine, 4, 1, 1-7.
Rosenstock, J., & Owens, D. (January 01, 2008). Treatment of Type 2 Using Insulin: When to Introduce?.
Ruffin, T. R. (January 01, 2016). Health Information Technology and Change.
Stults-Kolehmainen, M. A., & Sinha, R. (January 01, 2014). The Effects of Stress on Physical Activity and Exercise. Sports Medicine, 44, 1, 81-121.
Valencia, W. M., &Florez, H. (January 01, 2014). Pharmacological treatment of diabetes in older people. Diabetes, Obesity & Metabolism, 16, 12, 1192-203.
Zoepke, A., & Green, B. (January 01, 2012). Diabetes and diabetic foot ulcers : an often hidden problem : general review. Wound Healing Southern Africa, 5, 1, 19-22.