Order Instructions:
Assignment Instructions
• You will each choose 3 different journal published research study articles that explain the patient’s behavioral and/or psychological responses to having the illness. Do not include articles discussing the physiology or pharmacology of the illness, treatment of the illness or behavioral/psychological responses, or the risk factors for first developing the illness.
• Locate relevant journal published research study articles (these articles need to have been written after 1997 and you must NOT use general literature review articles.
• Choose the 3 articles that best relate to your case study patient.
• Briefly summaries the main topic and focus of each study and include a very summary of the study’s methodology, results, and discussion (i.e. where the authors explain the reasons for their findings and research conclusions) for the articles;
• discuss how each article explicitly and specifically explains the behavioral and psychological responses that the patient in your case study is experiencing in response to their illness.
• Make sure you are using article databases such as PsycINFO, MEDLINE, and CINAHL to run your searches. PsycINFO is likely to find you the most relevant articles for this assignment and all assignments within the behavioral stream. Just using Google or Google Scholar will NOT find you the articles you need. Also, make sure that the search terms you are using will give the databases the best chance of returning the articles you want. If you get no results with one search term, then try another or try and think laterally (e.g. what might be another word for “aggression” that you might find in the literature… hint: what about “irritability”? Or another word for “anxiety” might be “fear” etc.).
• The articles you include must have been published in a journal. Do not include theses, magazines, books or book chapters, letter to the editor or news articles. Academic journals publish all sorts of articles including research studies, book reviews, general literature reviews, editorials/commentaries, letters) but for the articles you include in your Annotated Bibliography you need to use only research study articles. A research study article will describe in detail a qualitative or quantitative research study (e.g., an experiment) including information about the study’s methodology, results, discussion and conclusions. For example, the Module 1 reading Zeilani and Seymour (2012) qualifies as a research study article because the authors describe how they collected and analyzed their data. A Module 3 reading, Lusk and Lash (2005) is a general literature review and does not qualify as a research study as the author does not specify how they went about sourcing information for their article. Lusk and Lash’s article is still a credible and valid source of reference information but it is not a research study and so cannot be used in the Annotated Bibliography assignment.
SAMPLE ANSWER
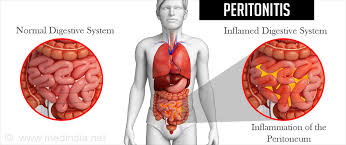
Peritonitis is a health condition that involves the inflammation of peritoneum (thin protective tissue layer that underlie the abdomen). This health condition is caused by infection which spreads around the body. It requires immediate treatment to prevent fatal complications from arising. In patients who have undergone surgical treatment, autonomic responses, mood swings and psychological coping responses are common. This paper explores 3 different journal study articles that explain patient’s behavioral and psychological responses to this illness. This study focuses on behavioral and psychosocial responses following surgical responses.
Boer, K. R., Mahler, C. W., Unlu, C., Lamme, B., Vroom, M. B., Sprangers, M. A., … Boermeester, M. A. (2007). Long-term prevalence of post-traumatic stress disorder symptoms in patients after secondary peritonitis. Critical Care, 11(1), R30.
Introduction/Literature review: This study investigates the behavioral response following secondary peritonitis. This is because numerous hospital admissions and intensive care unit (ICU) can be physically, emotionally and financially exhaustive. Patients who survive critical illness report critical poor quality of live and symptomology (PTSD) such as numbing, anxiety, loss of avoidant and intrusive recollections. The study suggests that the behavioral interventions are vital in patients with secondary peritonitis.
Methodology: This is a retrospective cohort in patients diagnosed with secondary peritonitis. The study comprises of 278 patients who had undergone surgery for secondary peritonitis, where 131 of them were long term survivors. The patients were interviewed Post-traumatic Stress Syndrome 10-question inventory (PTSS-10).
Study/ Results: The study indicates that in a cohort of 100 patients diagnosed with secondary peritonitis, 86% of them presented with post traumatic stress disorder. PTSD related symptoms were also present in 4.3 times higher in older male patients.
Discussion/explanation: The study indicates that 25% patients who have received surgical treatment for peritonitis are likely to be emotionally and physically upset due to surgical-related trauma, which could exacerbate illness behavior. The study suggests that patterns of behavior are seen as a product of socio-cultural conditioning and coping strategies. The study suggests that healthcare providers should recognize patient’s responses to various health procedures associated with pain and anxiety. Other symptoms such as impaired appetite, lack of energy and disturbed sleep can occur due to illness. In addition, some treatments can affect patient’s mood. These conditions can also be aggravated by other environmental factors such as financial strain of lack of physical and emotional support.
Application to the case study: The study findings contribute to the body of research that demonstrates that psychosocial responses in patients are associated with the socio-cultural factors. The suggests that the healthcare providers should incorporate psychosocial interventions in routine care so as to help patients such as Mr. Jacobs to manage stress associated with their new lifestyles of dependency, helplessness and pain. It is important for the healthcare providers to identify and be aware of this hidden morbidity among the patients diagnosed with secondary peritonitis.
Jennifer Finnegan-John and Veronica J. Thomas, “The Psychosocial Experience of Patients with End-Stage Renal Disease and Its Impact on Quality of Life: Findings from a Needs Assessment to Shape a Service,” ISRN Nephrology, vol. 2013, Article ID 308986, 8 pages, 2013. doi:10.5402/2013/308986
Introduction/Literature review: This study investigates the psychosocial experiences in patients with end stage renal disease. The study conducts needs assessment on renal patients to explore their psychological, spiritual and social needs. The study objective was to investigate behavioral responses and to conduct needs assessment so as to develop a comprehensive health psychology that can run concurrently with renal counseling.
Methodology: The study design is prospective qualitative. The study population consisted of 50 patients with end stage renal disease. The mean age of the participants was 55 years and 40% of them were from black and minority ethnic group. The study utilized series of semi- structured face to face interviews in renal patients and their carers in order to explore their behavioral and psychological responses and how the disease impacted their quality of life.
Study/ Results: The study findings indicated that depressive symptoms and disruptive behaviors are common in renal patients. This is associated with the psychological burden associated with the disease. Most of the patients in the study had feelings associated with depression and anxiety.
Discussion/explanation: This retrospective study indicates that depression and anxiety is a common behavioral response in patient diagnosed with renal disease. The study suggests that about 25% of patients who are diagnosed with the disease suffer from psychological burden. This behavioral response is associated with emotional numbness, avoidance of social activities and events. It is also associated difficulty in sleeping, disruptive and reckless behavior and is easily irritated. The study states that these are body responses to stress or perceived threat.
Application to the case study: The study indicates that depression and anxiety is a behavioral response that goes beyond the mental health. Based on this study, Mr. Jacob’s behavioral responses (irritability, social isolation and binge drinking) could be associated with the emotional burden of the disease. This research is interesting because it suggests that healthcare providers should engage with psychiatrists to help them better manage their improved outcome health.
Mckercher, C.M., Venn, A.J., Blizzard, L., Nelson, M., Palmer, A., Sshby, M., Scott, J., and Jose. M.D. (2012). Psychosocial factors in adults with chronic kidney disease: characteristics of pilot participants in the Tasmanian Chronic Kidney Disease study. BMC Nephrology, 14:83DOI: 10.1186/1471-2369-14-83
Introduction/Literature review: This study investigates behavioral and psychosocial responses in patient diagnosed with chronic illness. The literature links health outcomes with depression, anxiety and dispositional tendency described by aggression, cynicism attitudes and anger/irritability. The study also indicates that hostility, anger and depression are related with renal failure experiences. According to this study, these psychosocial responses are controlled by biomedical risk factors, and are associated with most aspects of immune function.
Methodology: This study design is quantitative. The study consisted of 105 patients above 18 years diagnosed with stage 4 CKD and was not under dialysis. The measures used in this study include depression (9- item patient Health questionnaire) and Beck Anxiety Inventory to investigate behavioral responses with disease progression and patient’s quality of life.
Study/ Results: The study findings indicated that hostility and patient’s behavioral responses to chronic disease are correlated with their plasma levels of CRP. The study findings indicated that the cycle of inflammation levels influence depressive behavior, indicating that depression is problematic indicator of patients under chronic pain.
Discussion/explanation: The longitudinal study findings indicated that there is a relationship between the CRP levels and psychosocial factors. The study also states that hormonal changes also induce inflammatory processes which in turn influence psychosocial responses. For instance, pain initiates systemic stress which activates neuro-endocrinological pathways (hypothalamic-pituitary-adrenal axis) leading to the secretion of stress hormone. Accumulation of stress hormone is associated with hostility and depressive symptoms. The study also suggests that genetic predispositions play a major role in both inflammation and hostility.
Application to the case study: The study findings contribute to the body of research that demonstrates that psychosocial responses in patients are associated with systemic inflammation. This indicates that the Mr. Jacob’s depressive behavior (irritability, social isolation and binge drinking) is associated with elevated levels of the systemic inflammation. This research is interesting because it suggests that healthcare providers should reduce systemic inflammation so as to improve patient’s ability to improve pain, and to help them cope with the illness-induced stress in their lives.
References
Boer, K. R., Mahler, C. W., Unlu, C., Lamme, B., Vroom, M. B., Sprangers, M. A., … Boermeester, M. A. (2007). Long-term prevalence of post-traumatic stress disorder symptoms in patients after secondary peritonitis. Critical Care, 11(1), R30. Retrieved from http://doi.org/10.1186/cc5710
Jennifer Finnegan-John and Veronica J. Thomas, “The Psychosocial Experience of Patients with End-Stage Renal Disease and Its Impact on Quality of Life: Findings from a Needs Assessment to Shape a Service,” ISRN Nephrology, vol. 2013, Article ID 308986, 8 pages, 2013. doi:10.5402/2013/308986
Mckercher, C.M., Venn, A.J., Blizzard, L., Nelson, M., Palmer, A., Sshby, M., Scott, J., and Jose. M.D. (2012). Psychosocial factors in adults with chronic kidney disease: characteristics of pilot participants in the Tasmanian Chronic Kidney Disease study. BMC Nephrology, 14:83DOI: 10.1186/1471-2369-14-83
We can write this or a similar paper for you! Simply fill the order form!